Arrhythmias are abnormal heart rhythms that can lead to various health complications. In some cases, these conditions necessitate the implantation of a pacemaker, a device designed to regulate the heart’s rhythm. This article will explore the types of arrhythmias that may require a pacemaker, detailing their characteristics, symptoms, and the rationale behind using a pacemaker as a treatment option.
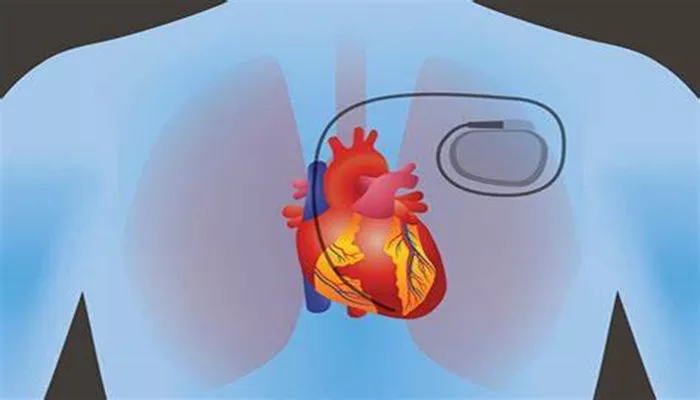
What Is A Pacemaker?
A pacemaker is a small, battery-operated device that helps manage heart rhythms. It sends electrical impulses to the heart to ensure it beats at a normal rate. Pacemakers can be classified into different types based on their functionality:
Single-Chamber Pacemaker: Connects to one chamber of the heart, usually the right ventricle.
Dual-Chamber Pacemaker: Connects to both the right atrium and right ventricle, coordinating contractions between these chambers.
SEE ALSO: How to Read Sinus Arrhythmia ECG?
Biventricular Pacemaker: Also known as cardiac resynchronization therapy (CRT), this device connects to both ventricles and is used primarily in patients with heart failure to improve synchronization of heart contractions.
Types of Arrhythmias Requiring A Pacemaker
Several arrhythmias can lead to the need for a pacemaker. Below is a detailed summary of these conditions:
1. Sinus Node Dysfunction (SND)
Sinus node dysfunction occurs when the heart’s natural pacemaker (the sinus node) fails to function properly. This can lead to bradycardia (slow heart rate) or pauses in heartbeats. Symptoms may include:
- Fatigue
- Dizziness
- Fainting spells
A pacemaker is often indicated in cases where patients experience significant symptoms due to SND.
2. Atrioventricular (AV) Block
AV block occurs when electrical signals between the atria and ventricles are delayed or blocked. There are three degrees of AV block:
First-Degree AV Block: Mild delay in conduction; often asymptomatic and may not require treatment.
Second-Degree AV Block: Occurs when some signals are blocked; type II (Mobitz type II) is particularly concerning as it can progress to complete block.
Third-Degree AV Block: Complete block where no signals reach the ventricles; this condition is critical and usually requires immediate pacing.
Patients with symptomatic second-degree or third-degree AV block typically benefit from pacemaker implantation to restore normal rhythm and prevent complications such as syncope.
3. Chronic Atrial Fibrillation with Slow Ventricular Response
In patients with atrial fibrillation, if the ventricular response is too slow (often due to medication or underlying conduction system disease), it may lead to inadequate blood flow and symptoms like fatigue or dizziness. A dual-chamber pacemaker can help maintain an appropriate heart rate during these episodes.
4. Sustained Ventricular Tachycardia (VT)
Sustained VT can be life-threatening if it leads to hemodynamic instability. In certain cases, especially when associated with pauses or bradycardia, a pacemaker may be used in conjunction with an implantable cardioverter-defibrillator (ICD) for better management of these arrhythmias.
5. Neurocardiogenic Syncope
Neurocardiogenic syncope refers to fainting spells caused by sudden drops in heart rate or blood pressure. In patients who experience recurrent syncope due to significant bradycardia or asystole (temporary cessation of heartbeat), a pacemaker may be indicated as a preventive measure.
6. Congenital Heart Disease
Certain congenital heart defects can disrupt normal electrical conduction pathways, leading to arrhythmias that may require pacing.
For example, patients with complete atrioventricular septal defects may develop complete heart block and need permanent pacing.
7. Cardiac Resynchronization Therapy (CRT)
Patients with heart failure who exhibit ventricular dyssynchrony—where the left and right ventricles do not contract simultaneously—may benefit from CRT using a biventricular pacemaker. This therapy improves cardiac output and reduces symptoms associated with heart failure.
Indications for Pacemaker Implantation
The decision to implant a pacemaker is guided by clinical indications categorized into three classes by the American College of Cardiology (ACC), American Heart Association (AHA), and Heart Rhythm Society (HRS):
Class I: Conditions where pacemaker implantation is indicated and beneficial.
Class II: Situations where there is conflicting evidence regarding efficacy; further evaluation may be needed.
Class III: Conditions where pacing is not recommended due to potential harm.
Conclusion
Pacemakers play a crucial role in managing various arrhythmias that can significantly impact patient health and quality of life. Conditions such as sinus node dysfunction, AV block, chronic atrial fibrillation with slow ventricular response, sustained VT, neurocardiogenic syncope, congenital heart disease, and severe heart failure are among those that may necessitate pacing intervention.
The decision for implantation involves careful consideration of symptoms, underlying conditions, and potential benefits versus risks associated with the procedure. As technology advances, the effectiveness and safety of pacemakers continue to improve, offering hope for many patients suffering from arrhythmias.
Related topics: