Occlusive coronary artery sclerosis, commonly referred to as coronary artery disease (CAD), is a significant health concern that affects millions of people worldwide. This condition is characterized by the narrowing or blockage of the coronary arteries, which supply oxygen-rich blood to the heart muscle. The primary cause of this condition is the buildup of plaque within the arteries, leading to various complications, including angina, heart attacks, and heart failure. This article aims to provide a comprehensive overview of occlusive coronary artery sclerosis, its causes, symptoms, diagnosis, treatment options, and prevention strategies.
What Is Coronary Artery Disease?
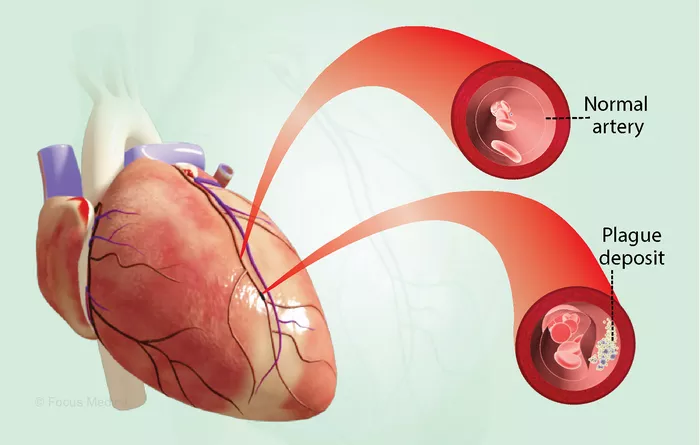
Coronary artery disease occurs when the coronary arteries become narrowed or blocked due to atherosclerosis.
Atherosclerosis is a process where fatty deposits, cholesterol, and other substances accumulate on the artery walls, forming plaques. Over time, these plaques can harden and restrict blood flow to the heart muscle.
Pathophysiology of Atherosclerosis
The development of atherosclerosis begins with damage to the endothelium, the inner lining of the arteries. This damage can be caused by various factors such as high blood pressure, smoking, high cholesterol levels, and diabetes. Once the endothelium is compromised, low-density lipoprotein (LDL) cholesterol can infiltrate the arterial wall.
As LDL cholesterol accumulates, it triggers an inflammatory response that attracts white blood cells to the site. These immune cells attempt to engulf the cholesterol but may become engorged and form foam cells. Over time, foam cells accumulate and contribute to plaque formation. As plaques grow larger, they can cause significant narrowing of the artery lumen, leading to reduced blood flow.
Risk Factors for Coronary Artery Disease
Several risk factors contribute to the development of occlusive coronary artery sclerosis:
Age: The risk increases with age; men over 45 and women over 55 are at higher risk.
Family History: A family history of heart disease can increase an individual’s risk.
Smoking: Tobacco use damages blood vessels and accelerates atherosclerosis.
High Blood Pressure: Hypertension can damage arteries over time.
High Cholesterol Levels: Elevated LDL cholesterol contributes to plaque buildup.
Diabetes: High blood sugar levels can damage blood vessels and increase plaque formation.
Obesity: Excess weight increases the risk of high blood pressure and diabetes.
Physical Inactivity: A sedentary lifestyle contributes to obesity and other risk factors.
Unhealthy Diet: Diets high in saturated fats, trans fats, and cholesterol can increase cholesterol levels.
Symptoms of Coronary Artery Disease
Many individuals with CAD may not experience symptoms until significant blockage occurs. Common symptoms include:
Angina: Chest pain or discomfort that may feel like pressure or squeezing. It often occurs during physical exertion or emotional stress.
Shortness of Breath: Difficulty breathing during physical activity or even at rest in advanced cases.
Fatigue: Unusual tiredness or lack of energy can occur due to inadequate blood flow.
Heart Attack Symptoms: Severe chest pain that lasts more than a few minutes or goes away and comes back; pain may radiate to the arms, neck, jaw, or back.
Diagnosis of Coronary Artery Disease
Diagnosing CAD involves several steps:
Medical History Review: A healthcare provider will assess symptoms and personal/family medical history.
Physical Examination: A thorough examination may reveal signs such as high blood pressure or abnormal heart sounds.
Diagnostic Tests:
Electrocardiogram (ECG): Measures electrical activity in the heart; abnormalities may indicate CAD.
Stress Testing: Monitors heart function during physical exertion.
Echocardiogram: Uses sound waves to create images of the heart’s structure and function.
Coronary Angiography: Involves injecting dye into coronary arteries to visualize blockages through X-ray imaging.
Treatment Options for Coronary Artery Disease
Treatment for CAD aims to relieve symptoms, prevent complications, and improve quality of life. Options include:
Lifestyle Modifications
Making healthy lifestyle changes is crucial in managing CAD:
Diet: Adopting a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help lower cholesterol levels.
Exercise: Regular physical activity strengthens the heart and improves circulation.
Weight Management: Achieving a healthy weight reduces strain on the heart.
Smoking Cessation: Quitting smoking significantly lowers cardiovascular risks.
Medications
Several medications may be prescribed to manage CAD:
Antiplatelet Agents: Aspirin or clopidogrel helps prevent blood clots.
Statins: These drugs lower LDL cholesterol levels and stabilize plaques.
Beta-blockers: Reduce heart rate and lower blood pressure.
ACE Inhibitors: Help relax blood vessels and lower blood pressure.
Medical Procedures
In some cases, medical procedures may be necessary:
Angioplasty and Stenting: A catheter is used to widen narrowed arteries; a stent may be placed to keep them open.
Coronary Artery Bypass Grafting (CABG): Surgery reroutes blood around blocked arteries using grafts from other parts of the body.
Complications Associated with Coronary Artery Disease
If left untreated or poorly managed, CAD can lead to severe complications:
Heart Attack (Myocardial Infarction): Occurs when blood flow to part of the heart is blocked for an extended period.
Heart Failure: The heart becomes unable to pump enough blood to meet the body’s needs due to weakened muscle from prolonged ischemia.
Arrhythmias: Abnormal heart rhythms can develop due to damaged heart tissue.
Prevention Strategies for Coronary Artery Disease
Preventing CAD involves addressing modifiable risk factors:
Maintain a healthy diet low in saturated fats and high in fiber.
Engage in regular physical activity—aim for at least 150 minutes of moderate exercise weekly.
Avoid tobacco use entirely; seek help if needed.
Manage stress through relaxation techniques such as meditation or yoga.
Regularly monitor blood pressure and cholesterol levels with healthcare providers.
Control diabetes effectively through diet, exercise, and medication if necessary.
Conclusion
Occlusive coronary artery sclerosis is a serious condition that requires attention due to its potential complications.
Understanding its causes, recognizing symptoms early on, seeking timely diagnosis, and adhering to treatment plans are vital steps in managing this disease effectively. By adopting healthier lifestyle choices and working closely with healthcare providers, individuals can significantly reduce their risk of developing coronary artery disease and improve their overall cardiovascular health.
Related topics:
- How Long Can You Live with Heart Valve Disease
- How Does Hypertension Cause Ischemic Heart Disease?
- How Long Can You Live with Mild Mitral Valve Regurgitation?