Torsades de Pointes (TdP) is a unique and critical arrhythmia that poses significant risks to patients, often leading to severe complications if not recognized and treated promptly. This article delves into the nature of TdP, its characteristics, underlying mechanisms, and the differences between TdP, ventricular tachycardia (VT), and ventricular fibrillation (VF).
Introduction
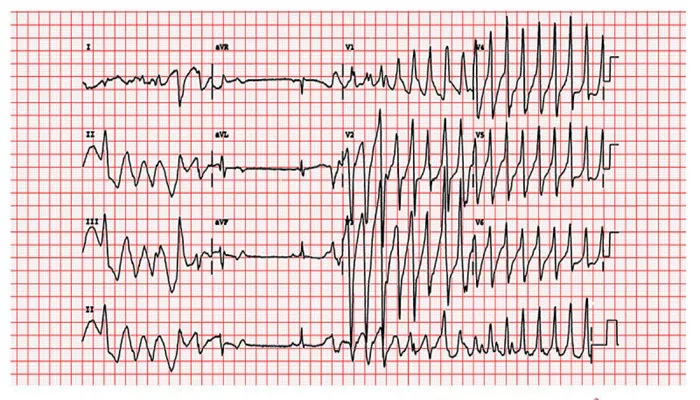
Torsades de Pointes translates from French as “twisting of the points,” which aptly describes the distinctive appearance of this arrhythmia on an electrocardiogram (ECG). TdP is classified as a polymorphic ventricular tachycardia, characterized by rapid and irregular QRS complexes that appear to twist around the baseline of the ECG. This phenomenon is often associated with a prolonged QT interval, which can be congenital or acquired due to various factors such as medications, electrolyte imbalances, or underlying heart conditions.
Understanding TdP is crucial for cardiologists and healthcare providers because it can lead to more severe arrhythmias, including ventricular fibrillation, which can result in sudden cardiac arrest.
What Is Torsades de Pointes?
Torsades de Pointes is a form of ventricular tachycardia that occurs in the context of a prolonged QT interval. The hallmark feature of TdP on an ECG is the oscillation of the QRS complexes around the isoelectric line, giving it a twisting appearance.
The heart rate during TdP typically ranges from 200 to 250 beats per minute. While TdP can resolve spontaneously, it has the potential to degenerate into ventricular fibrillation, a life-threatening condition where the heart’s electrical activity becomes chaotic, preventing effective blood circulation.
Pathophysiology of Torsades de Pointes
The underlying mechanism of TdP involves abnormalities in cardiac ion channels that regulate the heart’s electrical activity. Specifically, a prolonged QT interval results from either:
Loss of function in repolarizing potassium channels.
Gain of function in depolarizing sodium or calcium channels.
These disruptions lead to delayed repolarization and early after-depolarizations (EADs), which can trigger TdP when a premature ventricular contraction (PVC) occurs during the vulnerable period of repolarization—known as the R-on-T phenomenon. This phenomenon is critical in understanding how TdP can initiate and sustain itself.
Risk Factors for Torsades de Pointes
Several risk factors contribute to the development of TdP, including:
Congenital Long QT Syndrome: A genetic condition that predisposes individuals to prolonged QT intervals.
Medications: Certain drugs, including antiarrhythmics, antidepressants, and antibiotics, can prolong the QT interval.
Electrolyte Imbalances: Low levels of potassium (hypokalemia) or magnesium (hypomagnesemia) can increase susceptibility.
Bradycardia: Slow heart rates can exacerbate the risk.
Heart Conditions: Structural heart disease or previous myocardial infarction may also be contributing factors.
Symptoms And Diagnosis
Patients experiencing TdP may present with symptoms such as palpitations, dizziness, lightheadedness, syncope (fainting), or even cardiac arrest in severe cases. The diagnosis relies heavily on an ECG, which will show the characteristic twisting pattern of QRS complexes.
In some instances, TdP may be preceded by a series of short-long-short R-R intervals on the ECG.
Treatment Options for Torsades de Pointes
Management of TdP focuses on immediate stabilization and addressing underlying causes. Key treatment strategies include:
Magnesium Sulfate: Administered intravenously to help stabilize cardiac membranes.
Electrolyte Correction: Addressing any imbalances such as hypokalemia or hypomagnesemia.
Overdrive Pacing: In cases where TdP is recurrent or persistent, pacing may be employed to increase heart rate and shorten the QT interval.
Defibrillation: If TdP degenerates into ventricular fibrillation, immediate defibrillation is necessary.
Torsades de Pointes Vs. Ventricular Fibrillation
While both TdP and ventricular fibrillation are serious arrhythmias that can lead to sudden cardiac death, they differ significantly in their characteristics:
| Feature | Torsades de Pointes | Ventricular Fibrillation |
| Type | Polymorphic Ventricular Tachycardia | Chaotic Electrical Activity |
| ECG Appearance | Twisting QRS complexes | Irregular and chaotic waveforms |
| Heart Rate | 200-250 beats per minute | Very rapid and disorganized |
| Potential for Spontaneous Resolution | Yes | No |
| Treatment | Magnesium sulfate, pacing | Immediate defibrillation |
TdP can often resolve spontaneously but has the potential to progress into VF if not managed appropriately. In contrast, VF represents a state where there is no effective heartbeat due to disorganized electrical activity in the ventricles.
Conclusion
Torsades de Pointes is a critical arrhythmia that requires prompt recognition and intervention. Understanding its pathophysiology helps healthcare providers identify at-risk patients and implement appropriate treatment strategies. While it is classified as a form of ventricular tachycardia, its potential progression into ventricular fibrillation underscores its severity. Ongoing research into genetic predispositions and drug interactions continues to enhance our understanding and management of this dangerous condition.
In summary, Torsades de Pointes is not ventricular fibrillation but rather a specific type of polymorphic ventricular tachycardia that can lead to VF if not treated effectively. Awareness and education surrounding TdP are essential for improving patient outcomes and preventing sudden cardiac events associated with this arrhythmia.
Related topics:
- Why Does Hypokalemia Cause Arrhythmia?
- How Common Is Respiratory Sinus Arrhythmia?
- What Arrhythmia Treatments Do Electrophysiologists Provide