Right-sided heart failure, also known as right ventricular failure, occurs when the right side of the heart is unable to pump blood effectively to the lungs. This condition can lead to a variety of complications and symptoms, significantly impacting a person’s quality of life. This article will explore the causes, symptoms, and complications associated with right-sided heart failure, providing a detailed overview for both healthcare professionals and patients.
Introduction to Right-Sided Heart Failure
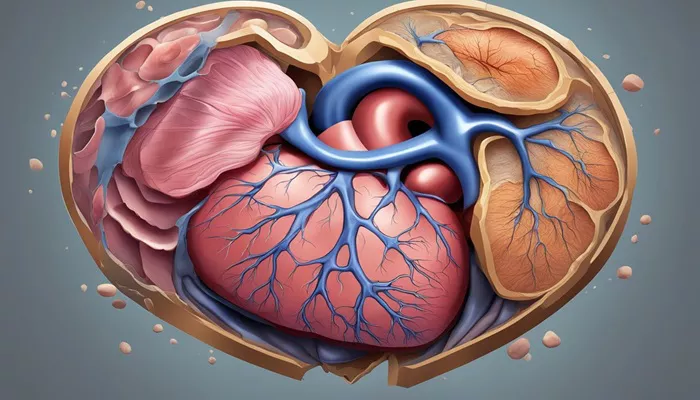
The heart functions as a pump, circulating blood throughout the body.
It consists of four chambers: two atria and two ventricles. The right side of the heart receives deoxygenated blood from the body through the superior and inferior vena cavae and pumps it to the lungs via the pulmonary arteries for oxygenation.
When the right ventricle fails, it cannot maintain adequate blood flow to the lungs, leading to increased pressure in the venous system and fluid accumulation in various tissues.
Right-sided heart failure is often secondary to left-sided heart failure, which is more common. When the left ventricle fails, it can cause a backlog of blood into the lungs, increasing pressure in the pulmonary circulation. Over time, this elevated pressure can strain the right ventricle, leading to its eventual failure. Other causes of right-sided heart failure include chronic lung diseases such as chronic obstructive pulmonary disease (COPD), pulmonary hypertension, valvular heart diseases, and congenital heart defects.
Causes of Right-Sided Heart Failure
Left-Sided Heart Failure: The most prevalent cause of right-sided heart failure is left-sided heart failure. When the left ventricle fails, blood backs up into the lungs, increasing pressure in the pulmonary arteries. This condition forces the right ventricle to work harder, eventually leading to its weakness and failure.
Chronic Lung Diseases: Conditions like COPD and pulmonary fibrosis can elevate pressure in the pulmonary arteries (pulmonary hypertension), making it difficult for the right ventricle to pump blood effectively.
Valvular Heart Disease: Disorders such as tricuspid regurgitation or pulmonic stenosis can obstruct blood flow from the right side of the heart, contributing to its failure.
Pulmonary Embolism: A blockage in one of the pulmonary arteries can suddenly increase pressure on the right side of the heart, potentially leading to acute right-sided heart failure.
Other Factors: Additional contributors include sleep apnea, high blood pressure, diabetes, obesity, and substance abuse (e.g., cocaine or excessive alcohol use) which can all strain cardiac function.
Symptoms of Right-Sided Heart Failure
The symptoms of right-sided heart failure can vary widely among individuals but typically include:
Swelling (Edema): Fluid retention leads to swelling in various parts of the body such as legs, ankles, abdomen (ascites), and sometimes even in internal organs.
Shortness of Breath: Patients may experience difficulty breathing during physical activity or when lying flat due to fluid accumulation.
Fatigue: As blood circulation becomes compromised, individuals often feel fatigued and lack energy due to insufficient oxygen delivery to tissues.
Chest Discomfort: Some patients report discomfort or pain in their chest areas as a result of increased pressure within the heart chambers.
Frequent Urination: Increased fluid retention may lead to more frequent urination at night (nocturia) as fluid shifts back into circulation while lying down.
Loss of Appetite and Nausea: The buildup of fluid in abdominal organs can cause feelings of fullness and nausea.
Weight Gain: Sudden weight gain due to fluid retention is common among individuals with right-sided heart failure.
Complications Associated with Right-Sided Heart Failure
Right-sided heart failure can lead to several serious complications that require medical attention:
Cardiac Cachexia: This condition refers to severe weight loss and muscle wasting that occurs due to chronic illness. Patients with advanced right-sided heart failure may experience significant loss of muscle mass and strength.
Organ Dysfunction: Prolonged fluid buildup can lead to dysfunction in organs such as the liver (congestive hepatopathy) and kidneys (renal insufficiency) due to decreased perfusion and increased pressure within these systems.
Pulmonary Hypertension: Chronic right-sided heart failure may contribute to or exacerbate pulmonary hypertension, creating a vicious cycle that further impairs cardiac function.
Arrhythmias: The strain on cardiac muscle can lead to electrical disturbances within the heart’s rhythm (arrhythmias), increasing risks for stroke or sudden cardiac death.
Conclusion
Right-sided heart failure is a complex condition that often arises from left-sided heart issues but can also stem from various other factors including lung diseases and valvular disorders. Its symptoms range from swelling and shortness of breath to fatigue and chest discomfort. Early diagnosis is crucial for effective management which includes medications, lifestyle changes, and possibly surgical interventions.
Understanding this condition’s implications allows healthcare providers and patients alike to approach treatment proactively, aiming not just for symptom relief but also for improved quality of life through comprehensive care strategies.
Regular follow-up with healthcare providers is essential for monitoring progression and adjusting treatment plans accordingly.
Related topics:
- What Stage of Heart Failure Is Shortness of Breath?
- How Long Can A Dog Live with Ascites Congestive Heart Failure
- How Does Hypertension Cause Heart Failure?