Atrial tachycardia (AT) is a type of arrhythmia originating from the atria of the heart. It is characterized by a rapid and abnormal heart rhythm that originates from an ectopic focus within the atria, rather than from the sinoatrial (SA) node, which is the heart’s natural pacemaker. The condition is often diagnosed through an electrocardiogram (ECG), a non-invasive test that records the electrical activity of the heart. Recognizing atrial tachycardia on an ECG is crucial for proper diagnosis and treatment, as it can sometimes be mistaken for other forms of supraventricular tachycardia (SVT).
In this article, we will discuss how to identify atrial tachycardia on an ECG, including its typical features, diagnostic criteria, and how it differs from other types of arrhythmias.
What Is Atrial Tachycardia?
Atrial tachycardia is a supraventricular arrhythmia where the atria of the heart beat faster than normal. The rate of atrial impulses in AT typically ranges from 100 to 250 beats per minute (bpm), which is significantly higher than the normal sinus rhythm rate of 60-100 bpm. In atrial tachycardia, the electrical impulses originate from an abnormal focus or ectopic pacemaker within the atria, which overrides the SA node, causing a rapid and irregular heart rhythm.
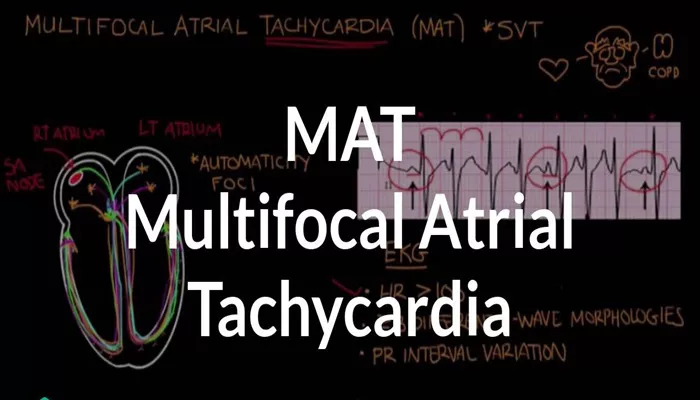
Atrial tachycardia can be classified into several subtypes, including focal, multifocal, and macro-reentrant AT, but the most common is focal atrial tachycardia, which arises from a single ectopic focus in the atrium.
Recognizing Atrial Tachycardia on an Electrocardiogram
An ECG is the most common and essential tool for diagnosing atrial tachycardia. It provides a visual representation of the electrical activity of the heart and helps physicians identify any abnormal rhythms or conduction problems. The main features of atrial tachycardia on an ECG include the following:
1. Rapid Heart Rate
One of the hallmark features of atrial tachycardia is a rapid heart rate. On the ECG, this is reflected in a tachycardic rhythm with a ventricular rate typically between 100 and 250 bpm. A rapid heart rate can cause the QRS complexes to become closely spaced, which can sometimes make it challenging to differentiate from other arrhythmias, such as atrial fibrillation (AF) or paroxysmal supraventricular tachycardia (PSVT).
2. Abnormal P-Waves
The most important distinguishing feature of atrial tachycardia is the abnormal P-waves. These are the electrical impulses originating from the atria that are recorded on the ECG before each QRS complex. In atrial tachycardia, the P-waves may appear differently than normal sinus P-waves, as they arise from an ectopic focus within the atria.
Morphology: The P-waves may be inverted, or they may have an abnormal shape depending on the location of the ectopic focus. In focal atrial tachycardia, the P-wave morphology can often be different from sinus P-waves and may appear as positive or negative deflections in the leads where the ectopic focus is active.
Premature P-Waves: In some cases, the P-waves may be prematurely triggered, occurring before the expected time.
3. P-Wave to QRS Relationship
Another important feature of atrial tachycardia is the relationship between the P-waves and the QRS complexes. In most cases, the P-waves occur just before the QRS complex, but there may be varying degrees of PR interval shortening depending on the specific type of AT.
The P-waves typically have a fixed relationship with the QRS complexes, meaning that each P-wave is followed by a QRS complex.
Fixed P-R Interval: In atrial tachycardia, the P-R interval (the time from the onset of the P-wave to the beginning of the QRS complex) is generally consistent and does not vary like it might in atrial fibrillation or other arrhythmias.
4. QRS Complexes
The QRS complexes in atrial tachycardia are typically narrow unless there is a pre-existing bundle branch block or an additional conduction abnormality. This is a key feature that differentiates atrial tachycardia from ventricular arrhythmias, which typically present with wide QRS complexes.
In most cases, the QRS complex is narrow because the impulses are conducted through the normal His-Purkinje system. If there is an aberrant conduction pathway or bundle branch block, the QRS complexes may become wide.
5. Regularity of Rhythm
Atrial tachycardia is typically a regular arrhythmia, meaning the P-P intervals (the time between consecutive P-waves) are consistent. This regularity is another feature that helps differentiate atrial tachycardia from atrial fibrillation, which is irregularly irregular.
However, in some cases, the rhythm may be slightly irregular due to varying atrial conduction times or ectopic foci within the atrium. These variations might result in a slightly irregular rhythm, but overall, atrial tachycardia tends to be more regular than other arrhythmias like atrial fibrillation.
6. Duration of the Arrhythmia
Atrial tachycardia can be paroxysmal, occurring in episodes that start and stop suddenly, or it can be persistent. On an ECG, the duration of the tachycardia episode can vary, with some episodes lasting for a few seconds or minutes, while others may last for hours or more.
Persistent atrial tachycardia may show signs of atrial remodeling on the ECG, and in cases of long-standing arrhythmias, the P-wave morphology may evolve.
Differentiating Atrial Tachycardia from Other Arrhythmias
It is important to distinguish atrial tachycardia from other forms of supraventricular tachycardia (SVT), as treatment approaches may differ. The most common arrhythmias that are confused with atrial tachycardia include:
Atrial Fibrillation (AF)
Atrial fibrillation is a highly irregular arrhythmia with no distinct P-waves. Instead, there is chaotic electrical activity in the atria, resulting in a wavy baseline or fibrillatory waves on the ECG. The ventricular response in AF is also irregular, unlike the regular rhythm seen in atrial tachycardia.
Paroxysmal Supraventricular Tachycardia (PSVT)
PSVT is another type of arrhythmia that originates above the ventricles. It is often characterized by a narrow QRS complex and a regular rhythm, similar to atrial tachycardia. However, PSVT is usually associated with a sudden onset and termination, and the P-waves may be hidden in the QRS complex or occur after the QRS complex, making it difficult to distinguish them.
Atrial Flutter
Atrial flutter is another arrhythmia that originates from the atria, but it is characterized by a very regular rhythm and a distinctive “sawtooth” pattern of P-waves. The ventricular response is often 2:1, 3:1, or 4:1 to the atrial impulses. Unlike atrial tachycardia, where P-waves are less uniform, atrial flutter presents with a consistent, rapid atrial rate, usually between 250 and 350 bpm.
Ventricular Tachycardia
Although ventricular tachycardia (VT) is not a supraventricular arrhythmia, it is important to differentiate it from atrial tachycardia, as VT typically presents with wide QRS complexes, whereas atrial tachycardia has narrow QRS complexes. VT is a much more dangerous arrhythmia, often requiring immediate medical intervention.
Conclusion
Atrial tachycardia is a type of arrhythmia that can be identified on an electrocardiogram through its characteristic features, including a rapid heart rate, abnormal P-waves, a fixed P-R interval, and narrow QRS complexes. Recognizing these signs is essential for accurate diagnosis and effective treatment, as atrial tachycardia can sometimes be mistaken for other types of arrhythmias.
Related topics: