Myocarditis is an inflammation of the heart muscle (myocardium) that can affect the heart’s ability to pump blood. It can be caused by viral infections, bacterial infections, autoimmune diseases, or exposure to toxins. Diagnosing myocarditis can be challenging due to its wide range of symptoms and overlap with other cardiovascular conditions. However, with careful attention to patient history, clinical signs, diagnostic tests, and imaging techniques, myocarditis can be detected early, improving treatment outcomes and preventing complications.
In this article, we will discuss the process of catching myocarditis, covering key diagnostic approaches, symptoms, and tools that healthcare providers use to identify this condition.
What Is Myocarditis?
Myocarditis refers to the inflammation of the myocardium, the middle layer of the heart’s walls, which contains heart muscle cells. This inflammation can affect the heart’s electrical and mechanical functions, leading to arrhythmias, heart failure, or even sudden cardiac death if left untreated.
Causes of Myocarditis
Viral Infections: The most common cause, with viruses such as Coxsackievirus, adenovirus, and parvovirus B19 being frequent culprits.
Bacterial Infections: Less common but can include pathogens such as Streptococcus and Staphylococcus.
Autoimmune Diseases: Conditions like lupus or rheumatoid arthritis can cause myocarditis due to immune system attacks on heart tissue.
Toxins and Drugs: Certain medications, illicit drugs, and alcohol can lead to myocarditis.
Other Infections: Fungal or parasitic infections, such as Chagas disease, can also cause myocarditis.
Symptoms of Myocarditis
The symptoms of myocarditis vary widely, ranging from mild to severe. Some individuals may not experience any symptoms at all, while others may suffer from acute heart failure. Common symptoms include:
Chest Pain: Often sharp or pressure-like, which can resemble a heart attack.
Fatigue: Extreme tiredness and weakness, sometimes progressing to difficulty performing everyday activities.
Shortness of Breath: Difficulty breathing, especially with physical activity or when lying flat.
Palpitations: Irregular heartbeats or a racing heart.
Swelling: Swelling in the legs, ankles, or feet due to fluid retention.
Fever: Often a sign of viral or bacterial infection leading to myocarditis.
Dizziness or Fainting: Lightheadedness or loss of consciousness due to impaired heart function.
Common Risk Factors
Viral Infections: Recent viral illnesses, especially those affecting the respiratory system.
Autoimmune Diseases: A history of autoimmune conditions.
Immunosuppressive Medications: Certain drugs used to manage autoimmune diseases or prevent organ rejection can increase susceptibility to myocarditis.
Age and Gender: Young adults, particularly men, are at higher risk.
How to Catch Myocarditis: Diagnosis
To diagnose myocarditis, doctors rely on a combination of patient history, clinical presentation, physical examination, and diagnostic tests. Here are the key steps in identifying myocarditis.
1. Detailed Patient History
A thorough history-taking is the first step in diagnosing myocarditis. Physicians will ask about:
Recent Viral or Bacterial Illness: Any recent symptoms of viral infections, such as a cold or flu, which may precede myocarditis.
Heart-Related Symptoms: Any chest pain, palpitations, or difficulty breathing.
Family History: A history of heart disease or sudden cardiac death in the family may raise suspicion.
Medication Use: Any medications, particularly immunosuppressants, which may contribute to myocarditis.
Other Risk Factors: Such as drug use, alcohol consumption, or a history of autoimmune diseases.
2. Physical Examination
During the physical exam, the doctor will assess the patient’s vital signs, including:
Heart Rate and Rhythm: Irregular heart rhythms (arrhythmias) may be present.
Blood Pressure: Low blood pressure may indicate heart failure.
Signs of Heart Failure: Swelling in the legs, fluid retention, or elevated neck veins can indicate that the heart is not pumping blood effectively.
Breathing Sounds: Crackling or abnormal lung sounds could indicate fluid buildup around the heart (pericardial effusion) or lungs (pulmonary edema).
3. Electrocardiogram (ECG or EKG)
An ECG is one of the most important tests for detecting myocarditis. It records the electrical activity of the heart and can show signs of inflammation, arrhythmias, or changes associated with heart failure. Common ECG findings in myocarditis include:
ST-T wave abnormalities: These may resemble those seen in heart attacks but are often more diffuse.
Prolonged PR interval: Suggesting impaired electrical conduction.
Ventricular arrhythmias: Irregular heart rhythms originating from the ventricles, which are common in myocarditis.
4. Blood Tests
Blood tests are crucial in assessing inflammation and heart injury. Key markers that may be elevated in myocarditis include:
Troponin: Elevated levels indicate damage to heart muscle cells.
Creatine Kinase (CK-MB): Another marker of heart muscle injury.
C-Reactive Protein (CRP): An inflammatory marker that can be elevated in myocarditis.
White Blood Cell Count: An increase may indicate an ongoing infection.
5. Echocardiogram (Heart Ultrasound)
An echocardiogram uses sound waves to create images of the heart and assess its function. In myocarditis, an echocardiogram can reveal:
Reduced Ejection Fraction: This indicates that the heart is not pumping blood efficiently.
Heart Wall Motion Abnormalities: Inflammation can affect specific regions of the heart muscle, leading to abnormal movement.
Pericardial Effusion: Fluid buildup around the heart due to inflammation.
6. Cardiac MRI (Magnetic Resonance Imaging)
Cardiac MRI is increasingly being used to diagnose myocarditis, as it can provide detailed images of the heart’s structure and function. MRI can help detect:
Myocardial Edema: Swelling of the heart muscle due to inflammation.
Late Gadolinium Enhancement: Areas of the heart that have been damaged by inflammation or scarring.
Pericardial Involvement: Fluid accumulation around the heart.
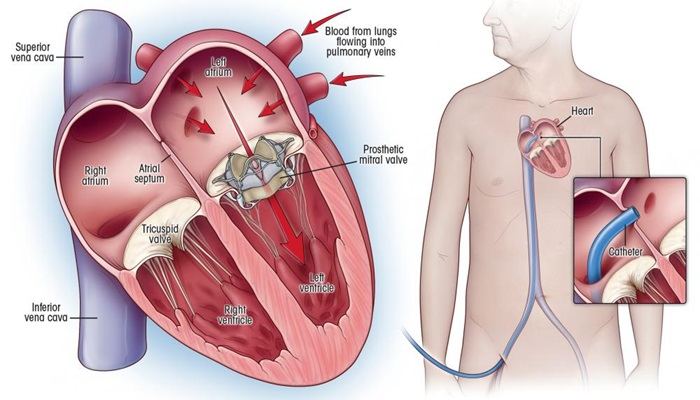
7. Endomyocardial Biopsy
In rare cases where the diagnosis is uncertain, an endomyocardial biopsy may be performed. This procedure involves removing a small sample of heart tissue for examination under a microscope. It is particularly useful for detecting viral infections or autoimmune causes of myocarditis.
However, due to its invasive nature, this test is usually reserved for severe cases or when other diagnostic methods are inconclusive.
8. Chest X-Ray
While not specific for myocarditis, a chest X-ray can help identify complications such as fluid buildup in the lungs (pulmonary edema) or an enlarged heart, which may suggest myocarditis or heart failure.
Differentiating Myocarditis from Other Conditions
Myocarditis shares symptoms with several other cardiac conditions, including:
Heart Attack (Myocardial Infarction): Chest pain and elevated troponin levels may suggest a heart attack, but an ECG and echocardiogram can help differentiate the two.
Pericarditis: Inflammation of the outer lining of the heart, which can present with chest pain similar to myocarditis but usually lacks heart failure symptoms.
Heart Failure: Chronic heart failure may present with fatigue and shortness of breath but without recent infection or inflammation.
Arrhythmias: Certain arrhythmias can present with palpitations and dizziness but do not necessarily indicate myocarditis.
9. Monitoring for Complications
Once myocarditis is suspected or diagnosed, it is crucial to monitor for complications, such as:
Heart Failure: Due to the heart’s reduced ability to pump blood.
Arrhythmias: Irregular heart rhythms, including life-threatening conditions like ventricular fibrillation.
Thromboembolic Events: Blood clots can form in the heart due to impaired heart function.
Conclusion
Myocarditis is a serious condition that requires early detection and proper management to prevent long-term damage to the heart. By combining patient history, physical examination, blood tests, imaging techniques, and, in some cases, tissue biopsy, healthcare providers can accurately diagnose myocarditis. If you or someone you know is experiencing symptoms such as chest pain, fatigue, or shortness of breath following a viral illness, it is crucial to seek medical attention promptly.
Early diagnosis and treatment can significantly improve the prognosis and prevent life-threatening complications.
Related topics: