Coronary Artery Disease (CAD) is one of the most prevalent cardiovascular conditions worldwide. It occurs when the blood vessels that supply the heart muscle with oxygen-rich blood—the coronary arteries—become narrowed or blocked. This restriction of blood flow can lead to a variety of complications, including chest pain, heart attacks, and even heart failure.
Homeostasis refers to the body’s ability to maintain a stable internal environment, which is essential for normal function. It involves a series of processes and feedback mechanisms that regulate the balance of various physiological parameters, such as temperature, pH, fluid balance, and blood pressure. When the body’s internal balance is disrupted, homeostasis is impaired, which can lead to disease or dysfunction.
In this article, we will explore how coronary artery disease (CAD) affects homeostasis and why it can have wide-reaching consequences on overall health. We will break down the effects of CAD on homeostasis by discussing how it impacts key physiological processes, such as oxygen delivery to tissues, blood pressure regulation, and the function of the heart.
The Impact of CAD on Oxygen Delivery to the Heart
A primary function of the coronary arteries is to provide oxygen and nutrients to the heart muscle (myocardium). When the coronary arteries are affected by CAD, the flow of oxygen-rich blood to the heart is compromised. This can lead to a condition known as ischemia, where the heart muscle does not receive enough oxygen to function effectively.
Ischemia disrupts the homeostatic balance within the body in several ways. When the heart muscle becomes oxygen-deprived, it cannot produce enough energy to contract properly. This leads to decreased cardiac output, which is the amount of blood the heart pumps per minute. Reduced cardiac output can lead to low blood pressure (hypotension) and insufficient blood flow to other vital organs.
The body tries to compensate for these changes by activating various homeostatic mechanisms. For example, the autonomic nervous system may increase heart rate (tachycardia) in an attempt to maintain an adequate cardiac output.
However, this can increase the heart’s demand for oxygen, exacerbating the ischemia. Over time, the compensatory mechanisms may become less effective, and the heart may suffer permanent damage, further disrupting homeostasis.
How CAD Affects Blood Pressure Regulation
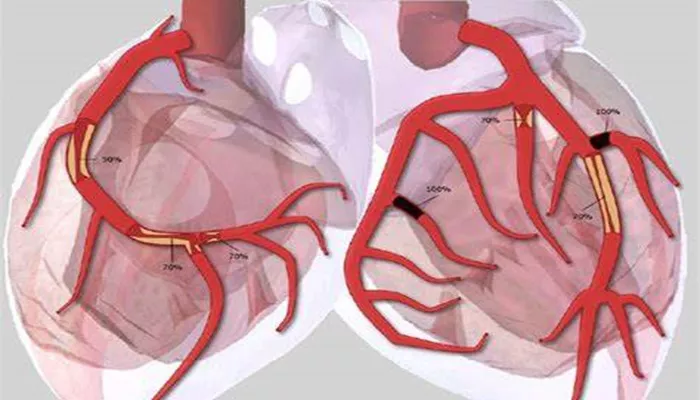
Blood pressure is a critical parameter in maintaining homeostasis. The blood vessels, including the coronary arteries, play a central role in regulating blood pressure by adjusting their diameter to control the flow of blood. When CAD is present, the coronary arteries become narrowed or blocked due to the buildup of plaque (atherosclerosis), which restricts blood flow.
This restriction affects blood pressure regulation in two primary ways:
Decreased Oxygen Supply to the Heart Muscle: As mentioned earlier, when the coronary arteries are narrowed, the heart muscle doesn’t get enough oxygen. This can lead to reduced cardiac output and lower blood pressure, which, in turn, can affect other organs and systems.
The kidneys, for instance, may sense a drop in blood pressure and activate the renin-angiotensin-aldosterone system (RAAS) to try to raise blood pressure. This system increases sodium and water retention, which increases blood volume and raises blood pressure.
Endothelial Dysfunction: The endothelial cells lining blood vessels play an important role in regulating blood pressure by releasing substances that either constrict or dilate blood vessels. In CAD, the endothelial cells can become damaged by the buildup of plaque and inflammation.
This damage impairs the ability of blood vessels to dilate properly, further contributing to high blood pressure (hypertension). Hypertension, in turn, puts additional strain on the heart and blood vessels, further impairing homeostasis.
The Effect of CAD on Fluid Balance
Fluid balance is another key aspect of homeostasis that can be disrupted by coronary artery disease. The heart plays a critical role in maintaining fluid balance by pumping blood through the kidneys, where excess fluid and waste products are filtered and excreted as urine.
When the heart is not pumping efficiently due to CAD-related ischemia or heart failure, the kidneys may not receive adequate blood flow.
This reduction in kidney perfusion can trigger a cascade of events that result in fluid retention. The kidneys may release more renin, which stimulates the production of angiotensin II and aldosterone. These hormones cause the kidneys to retain sodium and water, leading to an increase in blood volume. The retained fluid can accumulate in various parts of the body, causing edema (swelling), which can be seen in the legs, ankles, and lungs (pulmonary edema).
Pulmonary edema is particularly dangerous because it interferes with oxygen exchange in the lungs, worsening the heart’s ability to deliver oxygen to the tissues. This exacerbates the already compromised homeostasis, making it more difficult for the body to maintain normal function.
The Role of CAD in Inflammatory Response
Inflammation is a key part of the body’s immune response, but when it becomes chronic, it can lead to various health problems, including CAD. In CAD, the buildup of fatty deposits (plaque) in the coronary arteries triggers an inflammatory response. The body’s immune cells attempt to remove the plaque, but this process can cause further damage to the blood vessels and disrupt the delicate balance of homeostasis.
Inflammation can have several effects on the body:
Increased Blood Clotting: Inflammatory cytokines can increase the formation of blood clots, which can worsen the narrowing of the arteries. A blood clot in a coronary artery can completely block blood flow, leading to a heart attack. This acute event disrupts homeostasis by reducing oxygen supply to tissues, causing widespread tissue damage.
Increased Risk of Atherosclerosis Progression: Chronic inflammation accelerates the process of atherosclerosis, causing plaque to build up faster in the arteries. This leads to even greater restriction of blood flow and worsens the ischemia, further impairing homeostasis.
CAD And The Nervous System: A Complex Interaction
The nervous system is intimately involved in maintaining homeostasis, and CAD can influence its function in several ways.
The autonomic nervous system, which controls involuntary functions such as heart rate and blood pressure, is often overactivated in response to CAD. In an attempt to compensate for reduced blood flow and oxygen delivery, the sympathetic nervous system may release more adrenaline and norepinephrine, which increase heart rate and blood pressure.
While these compensatory mechanisms may initially help, they place additional stress on the heart and can worsen CAD over time.
Prolonged activation of the sympathetic nervous system can lead to heart arrhythmias, further disrupting normal heart function and homeostasis.
How CAD Leads to Long-Term Homeostatic Imbalance
Over time, the progression of coronary artery disease can lead to chronic imbalances in homeostasis. When blood flow to vital organs is compromised, tissues and organs begin to suffer from oxygen deprivation, leading to a cascade of effects that can impair overall health. For instance, the kidneys may become less efficient in regulating fluid balance, and the brain may not receive adequate oxygen, leading to cognitive dysfunction.
Additionally, the heart’s reduced ability to pump blood efficiently means that all systems in the body are affected, as they do not receive the nutrients and oxygen they need. This can manifest as shortness of breath, fatigue, muscle weakness, and swelling in various parts of the body.
Conclusion
Coronary artery disease is a condition that can profoundly affect the body’s homeostasis. By restricting blood flow to the heart, CAD impairs the ability of the heart to deliver oxygen and nutrients to tissues, disrupts blood pressure regulation, and causes fluid imbalances. The inflammatory response triggered by the buildup of plaque in the coronary arteries further complicates the situation, leading to increased clotting, accelerated atherosclerosis, and a greater risk of heart attack.
Related topics: