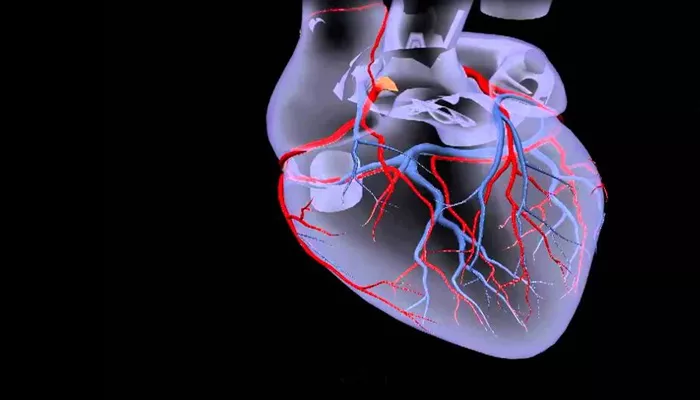
Coronary artery disease (CAD) is one of the leading causes of death worldwide. It refers to a condition in which the blood vessels that supply blood to the heart, known as coronary arteries, become narrowed or blocked. This can lead to a range of heart problems, including chest pain, heart attacks, and in severe cases, heart failure.
Understanding what coronary artery disease includes, its causes, symptoms, risk factors, diagnosis, and treatment options is crucial in managing and preventing this condition.
What Is Coronary Artery Disease?
Coronary artery disease (CAD) occurs when the coronary arteries, which supply oxygen and nutrients to the heart muscle, become damaged or diseased. The main cause of CAD is the buildup of plaque inside the arteries, a process known as atherosclerosis. Plaque is made up of cholesterol, fatty deposits, calcium, and other substances that circulate in the blood.
Over time, this plaque narrows the coronary arteries, reducing blood flow to the heart muscle.
When blood flow to the heart is restricted, the heart may not receive enough oxygen and nutrients to function properly.
This can lead to various symptoms, such as chest pain (angina), shortness of breath, or even a heart attack, where a part of the heart muscle is permanently damaged due to lack of oxygen.
Types of Coronary Artery Disease
Coronary artery disease can be categorized into several types based on the severity and nature of the condition:
1. Stable Angina
Stable angina is the most common form of CAD. It occurs when the heart is not getting enough oxygen, typically during physical activity or stress. The chest pain or discomfort is usually predictable and lasts for a short period. Rest or medication typically relieves the symptoms.
Stable angina is a sign that the coronary arteries are narrowed but not completely blocked.
2. Unstable Angina
Unstable angina is more serious and unpredictable. It can occur at rest or with minimal physical exertion. The pain is more intense and may last longer. Unstable angina can signal that a blood clot has partially or completely blocked a coronary artery, and it may lead to a heart attack if not treated promptly. It is considered a medical emergency and requires immediate attention.
3. Myocardial Infarction (Heart Attack)
A myocardial infarction (MI), commonly known as a heart attack, occurs when one or more of the coronary arteries become completely blocked, stopping blood flow to a part of the heart muscle. Without oxygen, the affected part of the heart muscle can begin to die. A heart attack often results in severe chest pain, shortness of breath, sweating, and nausea. Immediate medical intervention is required to restore blood flow and minimize heart damage.
4. Silent Myocardial Ischemia
Silent myocardial ischemia occurs when there is a reduction in blood flow to the heart muscle, but the person does not experience any noticeable symptoms, such as chest pain. It can lead to long-term damage to the heart muscle if not detected and treated. People with diabetes are more likely to experience silent myocardial ischemia.
5. Coronary Artery Spasm
A coronary artery spasm is a temporary reduction in blood flow caused by the tightening or narrowing of the coronary arteries. These spasms can occur without any plaque buildup and may result in chest pain or a heart attack. They can be triggered by stress, drug use (such as cocaine), or exposure to cold temperatures.
Causes of Coronary Artery Disease
The primary cause of coronary artery disease is atherosclerosis, a process that occurs over time due to the accumulation of plaque in the coronary arteries. Several factors contribute to this process:
1. High Cholesterol Levels
Elevated levels of low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol, contribute to plaque buildup. When LDL cholesterol is too high, it can get deposited along the walls of the arteries, leading to the formation of plaques.
2. High Blood Pressure (Hypertension)
High blood pressure damages the inner lining of the arteries, making it easier for plaque to build up. Over time, this increases the risk of developing CAD. Uncontrolled hypertension can also cause the heart to work harder, further increasing the risk of heart disease.
3. Smoking
Smoking is one of the most significant risk factors for coronary artery disease. The chemicals in cigarette smoke can damage the blood vessels, reduce oxygen levels in the blood, and promote the formation of blood clots, all of which increase the risk of CAD.
4. Diabetes
People with diabetes are at a higher risk for CAD because high blood sugar levels can damage the blood vessels and increase the likelihood of plaque buildup. Poorly controlled diabetes can lead to atherosclerosis and other cardiovascular problems.
5. Obesity
Being overweight or obese increases the risk of developing CAD due to its association with other risk factors, such as high cholesterol,
high blood pressure, and diabetes. Excess fat, especially abdominal fat, contributes to inflammation and increases the risk of heart disease.
6. Physical Inactivity
A sedentary lifestyle is another risk factor for CAD. Regular physical activity helps maintain a healthy weight, control blood pressure, improve cholesterol levels, and keep the heart and blood vessels in good condition.
7. Family History
A family history of coronary artery disease or heart disease increases a person’s risk of developing CAD. Genetics can play a role in how the body handles cholesterol and blood pressure, making some individuals more susceptible to heart disease.
8. Age
The risk of coronary artery disease increases with age. Men typically experience heart disease earlier than women, but after menopause, the risk in women increases significantly, reaching levels similar to men.
9. Stress
Chronic stress can lead to unhealthy behaviors such as smoking, overeating, and a lack of exercise, all of which contribute to the development of CAD. Stress also increases blood pressure and may have direct harmful effects on the heart and blood vessels.
Symptoms of Coronary Artery Disease
The symptoms of coronary artery disease can vary depending on the severity and type of CAD. Common symptoms include:
Chest pain (angina): Often described as a pressure, tightness, or heaviness in the chest. This can occur with physical activity or stress and is relieved by rest.
Shortness of breath: A feeling of breathlessness, particularly with exertion.
Fatigue: Unusual tiredness or lack of energy, especially during physical activity.
Dizziness or lightheadedness: Can occur when the heart is not pumping enough blood to the brain.
Nausea: Feeling nauseous, especially during a heart attack.
Pain in the arms, back, neck, or jaw: Pain radiating from the chest can also be felt in other areas of the upper body.
Not all individuals with CAD experience chest pain. Some people, especially those with diabetes or older adults, may have “silent” symptoms, where there are no obvious signs of heart disease.
Diagnosis of Coronary Artery Disease
Diagnosing coronary artery disease typically involves several steps:
1. Medical History and Physical Examination
The doctor will review the patient’s medical history, risk factors, and symptoms. A physical exam may include checking blood pressure, listening to the heart, and feeling for signs of fluid buildup.
2. Blood Tests
Blood tests are used to measure cholesterol levels, blood sugar, and other markers that may indicate an increased risk of heart disease.
3. Electrocardiogram (ECG)
An ECG records the electrical activity of the heart. It can identify abnormal heart rhythms, signs of previous heart attacks, or other issues related to CAD.
4. Stress Testing
A stress test involves exercising on a treadmill or bike while the heart is monitored. This helps evaluate how the heart responds to physical activity and may reveal areas of the heart that are not getting enough blood flow.
5. Echocardiogram
An echocardiogram uses sound waves to create images of the heart. It helps assess how well the heart is pumping and whether there is any damage to the heart muscle.
6. Coronary Angiography
Coronary angiography is a procedure in which a contrast dye is injected into the coronary arteries to create detailed X-ray images. This helps doctors identify blockages or narrowing in the arteries.
Treatment of Coronary Artery Disease
The treatment for coronary artery disease focuses on improving blood flow to the heart, managing symptoms, and reducing the risk of complications. Common treatments include:
1. Lifestyle Changes
Adopting a heart-healthy diet, engaging in regular exercise, quitting smoking, and managing stress are crucial in controlling risk factors for CAD.
2. Medications
Medications may be prescribed to lower cholesterol, control blood pressure, prevent blood clots, and relieve symptoms of angina.
3. Percutaneous Coronary Intervention (PCI)
PCI is a procedure that opens blocked arteries using a balloon or a stent. It is commonly referred to as angioplasty.
4. Coronary Artery Bypass Grafting (CABG)
CABG is a surgical procedure in which healthy blood vessels from other parts of the body are used to bypass blocked coronary arteries and restore blood flow to the heart.
Conclusion
Coronary artery disease is a serious condition that affects the blood vessels supplying the heart. It can lead to various heart problems, including angina, heart attacks, and heart failure. Understanding what CAD includes, its causes, symptoms, risk factors, and treatment options is essential for preventing and managing this condition. Early diagnosis and lifestyle changes, along with medical treatments, can help manage CAD and reduce the risk of complications.
Related topics: