Spontaneous intracranial hypotension (SIH) is a rare but debilitating condition characterized by low cerebrospinal fluid (CSF) pressure, resulting in a myriad of neurological symptoms. While the exact etiology of SIH remains elusive, researchers have made significant strides in elucidating the contributing factors to this perplexing disorder. This comprehensive article aims to explore the multifaceted nature of SIH, shedding light on its potential causes and underlying mechanisms.
Anatomy and Physiology of Cerebrospinal Fluid
Before delving into the complexities of SIH, it is crucial to grasp the fundamentals of cerebrospinal fluid (CSF) dynamics. CSF is a clear, colorless fluid that surrounds the brain and spinal cord, providing buoyancy, cushioning, and metabolic support to these vital structures. Produced primarily within the ventricles of the brain, CSF circulates throughout the central nervous system (CNS), exchanging nutrients and removing waste products.
Pathophysiology of Spontaneous Intracranial Hypotension
Spontaneous intracranial hypotension (SIH) arises when there is a disruption in the delicate equilibrium of CSF dynamics, leading to a decrease in intracranial pressure (ICP). This reduction in pressure can result from various mechanisms, including CSF leakages, impaired CSF production, or alterations in CSF absorption. The subsequent decline in ICP can trigger a cascade of neurological symptoms, ranging from headaches and nausea to more severe manifestations such as subdural hematomas and cranial nerve palsies.
Primary Causes of Spontaneous Intracranial Hypotension
While the precise cause of spontaneous intracranial hypotension (SIH) remains uncertain, several primary factors have been implicated in its pathogenesis. These include:
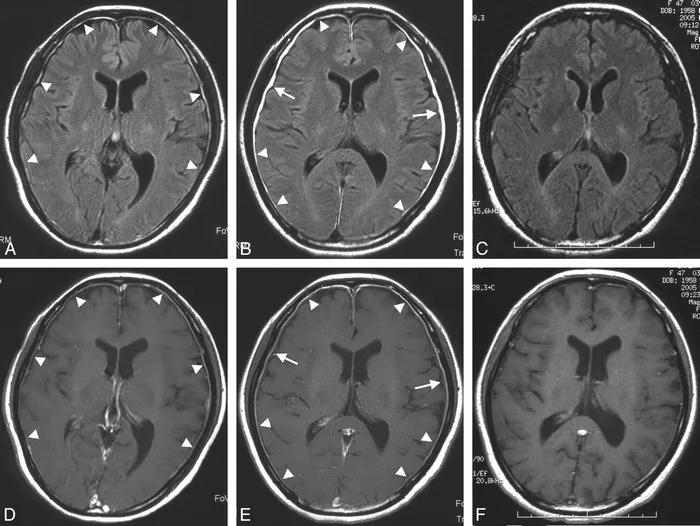
1. Dural Weakness and Spinal CSF Leakages: One of the leading hypotheses surrounding SIH involves dural weaknesses or defects that predispose individuals to spinal CSF leakages. These leaks can occur spontaneously or result from minor trauma, such as a sudden movement or strain. MRI imaging studies have revealed characteristic findings, such as diffuse pachymeningeal enhancement and subdural fluid collections, supporting the theory of CSF leaks as a primary cause of SIH.
2. Connective Tissue Disorders: There is growing evidence to suggest an association between connective tissue disorders (CTDs) and spontaneous intracranial hypotension (SIH). Conditions such as Ehlers-Danlos syndrome (EDS) and Marfan syndrome, characterized by abnormalities in collagen and elastin fibers, may predispose individuals to dural weaknesses and CSF leakages. Genetic studies have identified potential mutations in genes encoding extracellular matrix proteins, further implicating CTDs in the pathogenesis of SIH.
3. Obstructive Sleep Apnea: Emerging research has highlighted a potential link between obstructive sleep apnea (OSA) and spontaneous intracranial hypotension (SIH). The repetitive episodes of apnea and hypopnea characteristic of OSA can lead to fluctuations in intrathoracic pressure, ultimately impacting CSF dynamics. Additionally, the increased sympathetic activity associated with OSA may contribute to vascular engorgement and venous congestion, further exacerbating CSF leakages and hypotensive states.
Secondary Causes of Spontaneous Intracranial Hypotension
In addition to primary factors, several secondary causes may precipitate or exacerbate spontaneous intracranial hypotension (SIH). These include:
1. Iatrogenic Factors: Certain medical interventions, such as lumbar punctures, spinal surgeries, and epidural anesthesia, can inadvertently lead to CSF leakages and subsequent intracranial hypotension. While these procedures are often performed for diagnostic or therapeutic purposes, they carry inherent risks, particularly in individuals predisposed to dural weaknesses or connective tissue disorders.
2. Traumatic Spinal Injuries: Traumatic spinal injuries, including vertebral fractures and spinal cord contusions, can disrupt the integrity of the dural sac, resulting in CSF leakages and intracranial hypotension. These injuries may occur following motor vehicle accidents, falls, or sports-related trauma, highlighting the importance of vigilant monitoring and early intervention in affected individuals.
3. Idiopathic Intracranial Hypertension (IIH) Rebound: Idiopathic intracranial hypertension (IIH), characterized by elevated intracranial pressure (ICP) and papilledema, may paradoxically predispose individuals to spontaneous intracranial hypotension (SIH) following abrupt cessation of treatment. The withdrawal of medications such as acetazolamide or weight loss interventions can lead to rapid reductions in CSF production, exacerbating underlying CSF leakages and hypotensive states.
Diagnostic Evaluation and Management Strategies
The diagnosis of spontaneous intracranial hypotension (SIH) hinges on a comprehensive clinical assessment, augmented by neuroimaging studies and invasive procedures when necessary. Magnetic resonance imaging (MRI) remains the cornerstone of diagnostic imaging, with characteristic findings including diffuse pachymeningeal enhancement, subdural fluid collections, and descent of the brain within the cranial vault (brain sagging). In cases where imaging findings are equivocal or inconclusive, invasive procedures such as CT myelography or epidural blood patching may be required to confirm the diagnosis and localize CSF leakages.
Conclusion
Spontaneous intracranial hypotension (SIH) poses a formidable challenge to clinicians and researchers alike, owing to its diverse clinical manifestations and elusive pathogenesis. While the precise etiology of SIH remains incompletely understood, recent advancements in neuroimaging, genetics, and connective tissue biology have shed light on the multifaceted nature of this intriguing disorder. By elucidating the underlying factors contributing to SIH, clinicians can devise more effective diagnostic and therapeutic strategies, ultimately improving outcomes for affected individuals. Continued research efforts are warranted to unravel the intricate mechanisms driving CSF dynamics and to develop targeted interventions for this debilitating condition.