Congestive heart failure (CHF) is a serious medical condition that affects millions of people worldwide. It occurs when the heart is unable to pump enough blood to meet the body’s needs, leading to a buildup of fluid in the lungs and other parts of the body. This article will delve into the causes, symptoms, diagnosis, and treatment options for congestive heart failure, providing a comprehensive overview of this complex condition.
What is Congestive Heart Failure?
Congestive heart failure is a progressive condition that occurs when the heart muscle is weakened or damaged, leading to a decrease in its ability to pump blood effectively. As a result, blood may back up in the veins, causing fluid buildup in the lungs, abdomen, liver, and lower extremities. This fluid buildup is known as congestion, hence the term “congestive” heart failure.
Causes of Congestive Heart Failure
There are several underlying conditions and factors that can contribute to the development of congestive heart failure. These include:
1. Coronary Artery Disease (CAD): CAD is the most common cause of heart failure. It occurs when the arteries that supply blood to the heart become narrowed or blocked due to the buildup of plaque (atherosclerosis), reducing blood flow to the heart muscle.
2. High Blood Pressure (Hypertension): Chronic high blood pressure can strain the heart and lead to heart muscle thickening (hypertrophy) over time, eventually weakening the heart’s pumping ability.
3. Cardiomyopathy: This is a group of diseases that affect the heart muscle, causing it to become enlarged, thickened, or rigid. Cardiomyopathy can be genetic or acquired through factors such as viral infections, alcohol abuse, or certain medications.
4. Heart Valve Disorders: Malfunctioning heart valves, such as mitral valve prolapse or aortic stenosis, can disrupt normal blood flow through the heart, leading to heart failure.
5. Diabetes: Uncontrolled diabetes can damage blood vessels and nerves, increasing the risk of heart disease and heart failure.
6. Obesity: Excess body weight can strain the heart and increase the risk of developing conditions like high blood pressure, diabetes, and sleep apnea, all of which contribute to heart failure.
Symptoms of Congestive Heart Failure
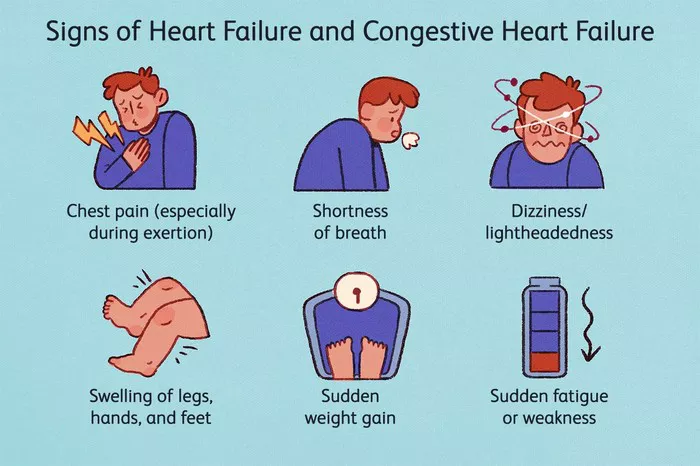
The symptoms of congestive heart failure can vary depending on the severity of the condition and which part of the heart is affected. Common symptoms include:
- Shortness of breath (especially during physical activity or when lying flat)
- Persistent coughing or wheezing
- Fatigue and weakness
- Swelling in the legs, ankles, feet, or abdomen (edema)
- Rapid or irregular heartbeat (palpitations)
- Reduced ability to exercise
- Increased need to urinate at night (nocturia)
- Sudden weight gain due to fluid retention
Diagnosis of Congestive Heart Failure
Diagnosing congestive heart failure typically involves a combination of medical history review, physical examination, and diagnostic tests. These may include:
1. Medical History and Physical Examination: Your doctor will ask about your symptoms, medical history, risk factors, and perform a physical exam to check for signs of heart failure such as fluid buildup, abnormal heart sounds, and swelling.
2. Blood Tests: Blood tests can help assess kidney function, electrolyte levels, and biomarkers such as B-type natriuretic peptide (BNP) or N-terminal pro-B-type natriuretic peptide (NT-proBNP), which are elevated in heart failure.
3. Imaging Tests: Various imaging techniques can provide detailed images of the heart and its function, including:
- Echocardiogram: Uses sound waves to create moving images of the heart’s structure and function.
- Electrocardiogram (ECG or EKG): Records the electrical activity of the heart to detect abnormalities.
- Cardiac MRI: Provides detailed images of the heart’s structure and function.
- Chest X-ray: Can show signs of fluid buildup in the lungs or heart enlargement.
4. Other Tests: Additional tests such as stress tests, cardiac catheterization, or coronary angiography may be performed to evaluate heart function, blood flow, and any blockages in the coronary arteries.
Treatment of Congestive Heart Failure
Treatment for congestive heart failure aims to improve symptoms, slow disease progression, and enhance quality of life. The specific treatment plan may vary depending on the underlying cause, severity of heart failure, and individual patient factors. Common treatment strategies include:
1. Lifestyle Modifications: This includes adopting a heart-healthy diet (low in sodium and saturated fats), engaging in regular physical activity, maintaining a healthy weight, limiting alcohol consumption, quitting smoking, and managing stress.
2. Medications: Several medications are used to manage heart failure symptoms and improve heart function, including:
- Angiotensin-Converting Enzyme (ACE) Inhibitors or Angiotensin II Receptor Blockers (ARBs): Help relax blood vessels and reduce strain on the heart.
- Beta-Blockers: Slow the heart rate and reduce blood pressure, improving heart function.
- Diuretics: Help remove excess fluid from the body, relieving symptoms of congestion.
- Aldosterone Antagonists: Help reduce fluid retention and improve heart function.
- Digoxin: Helps strengthen the heart’s contractions.
3. Device Therapy: In some cases, devices such as implantable cardioverter-defibrillators (ICDs) or cardiac resynchronization therapy (CRT) devices may be recommended to help regulate heart rhythm and improve pumping efficiency.
4. Surgery: Surgical procedures such as coronary artery bypass grafting (CABG), heart valve repair or replacement, or implantation of a ventricular assist device (VAD) or heart transplant may be necessary in advanced cases of heart failure.
5. Monitoring and Follow-Up: Regular monitoring of heart function, symptoms, medication adjustments, and lifestyle counseling are essential parts of managing congestive heart failure.
Conclusion
Congestive heart failure is a complex and potentially life-threatening condition that requires careful management and treatment. By understanding the causes, symptoms, diagnosis, and treatment options for heart failure, patients and healthcare providers can work together to improve outcomes and enhance quality of life for those affected by this condition. Early detection, lifestyle modifications, medication adherence, and regular medical follow-up are key components of a comprehensive approach to managing congestive heart failure and promoting heart health.