Left ventricular heart failure, also known as left-sided heart failure, is a condition where the left side of the heart is unable to pump blood effectively to meet the body’s needs. This can lead to a range of symptoms and complications, impacting a person’s quality of life and overall health. In this article, we will explore the various causes of left ventricular heart failure, including concrete cases to illustrate these causes.
1. Coronary Artery Disease (CAD):
One of the leading causes of left ventricular heart failure is coronary artery disease (CAD). CAD occurs when the arteries that supply blood to the heart muscle become narrowed or blocked due to the buildup of plaque. This reduces blood flow to the heart, leading to damage to the heart muscle over time. As a result, the left ventricle may weaken, affecting its ability to pump blood effectively.
Case Study: John, a 55-year-old man, presented with symptoms of chest pain and shortness of breath. Further investigations revealed significant blockages in his coronary arteries, leading to a diagnosis of CAD. Over time, the damage to his heart muscle resulted in left ventricular heart failure.
2. Hypertension (High Blood Pressure):
Chronic hypertension can also contribute to left ventricular heart failure. High blood pressure puts increased stress on the heart, causing the left ventricle to work harder to pump blood against the elevated pressure. This can lead to hypertrophy (thickening) of the heart muscle and eventually weaken the left ventricle.
Case Study: Sarah, a 60-year-old woman, had a history of uncontrolled hypertension for several years. Despite medication, her blood pressure remained high, leading to left ventricular hypertrophy. Over time, her heart’s ability to pump efficiently decreased, resulting in heart failure.
3. Valvular Heart Disease:
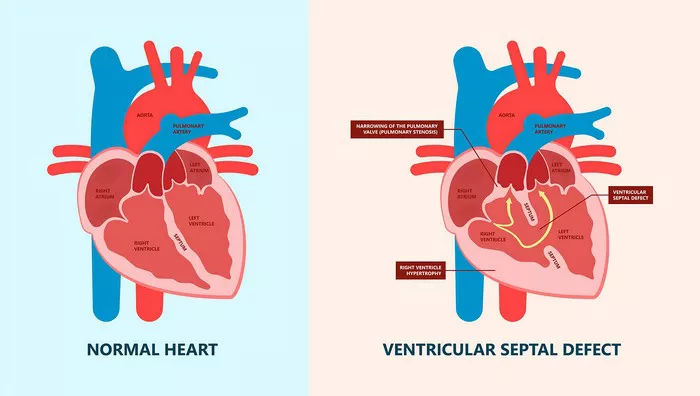
Malfunctioning heart valves can also contribute to left ventricular heart failure. Valvular heart disease, such as aortic stenosis (narrowing of the aortic valve) or mitral regurgitation (leaking of the mitral valve), can affect the left ventricle’s ability to function properly. This may lead to volume overload or pressure overload on the left ventricle, eventually causing heart failure.
Case Study: David, a 65-year-old man, was diagnosed with severe aortic stenosis. The narrowed aortic valve prevented adequate blood flow out of the left ventricle, leading to increased pressure and strain on the heart. Eventually, this resulted in left ventricular heart failure.
3. Myocardial Infarction (Heart Attack):
A myocardial infarction, commonly known as a heart attack, can cause damage to the heart muscle, including the left ventricle. When a coronary artery becomes blocked, depriving a portion of the heart muscle of oxygen-rich blood, it can lead to cell death and scarring. The damaged heart muscle may not function properly, contributing to heart failure.
Case Study: Emily, a 50-year-old woman, experienced a heart attack due to a blockage in one of her coronary arteries. The lack of blood flow to the affected area caused damage to her left ventricle, leading to impaired pumping function and eventual heart failure.
4. Cardiomyopathy:
Cardiomyopathy refers to diseases of the heart muscle, which can directly affect the left ventricle’s ability to pump blood effectively. Dilated cardiomyopathy, hypertrophic cardiomyopathy, and restrictive cardiomyopathy are examples of conditions that can lead to left ventricular heart failure.
Case Study: Michael, a 40-year-old man, was diagnosed with dilated cardiomyopathy, a condition where the heart muscle becomes stretched and weakened. This resulted in reduced contractility of the left ventricle, leading to heart failure symptoms such as fatigue and shortness of breath.
5. Arrhythmias:
Certain heart rhythm abnormalities, such as atrial fibrillation or ventricular tachycardia, can contribute to left ventricular heart failure. These arrhythmias can disrupt the heart’s normal pumping function, leading to inefficient blood circulation and potential damage to the left ventricle over time.
Case Study: Lisa, a 55-year-old woman, had a history of atrial fibrillation. The irregular heart rhythm caused episodes of rapid and inefficient contractions, affecting the left ventricle’s ability to fill and empty properly. This contributed to the development of left ventricular heart failure.
6. Infections and Inflammatory Conditions:
Infections such as myocarditis (inflammation of the heart muscle) or inflammatory conditions like systemic lupus erythematosus (SLE) can also lead to left ventricular heart failure. These conditions can cause direct damage to the heart muscle or trigger immune responses that affect cardiac function.
Case Study: James, a 30-year-old man, developed myocarditis following a viral infection. The inflammation in his heart muscle led to impaired left ventricular function, eventually progressing to heart failure.
Conclusion
Left ventricular heart failure can arise from various underlying causes, including coronary artery disease, hypertension, valvular heart disease, myocardial infarction, cardiomyopathy, arrhythmias, and infections/inflammatory conditions. These cases highlight the importance of early detection, proper management of risk factors, and targeted interventions to prevent or slow the progression of left ventricular heart failure.