Wolff-Parkinson-White Syndrome (WPW) is a cardiac condition characterized by an abnormality in the heart’s electrical system. While it may seem innocuous to some, WPW can be a dangerous condition that requires careful management and treatment. In this article, we will delve into the intricacies of WPW, exploring its underlying causes, potential complications, diagnostic methods, and treatment options. By gaining a deeper understanding of WPW, healthcare professionals and patients alike can work together to mitigate its risks and improve outcomes.
Understanding WPW: Causes and Mechanisms
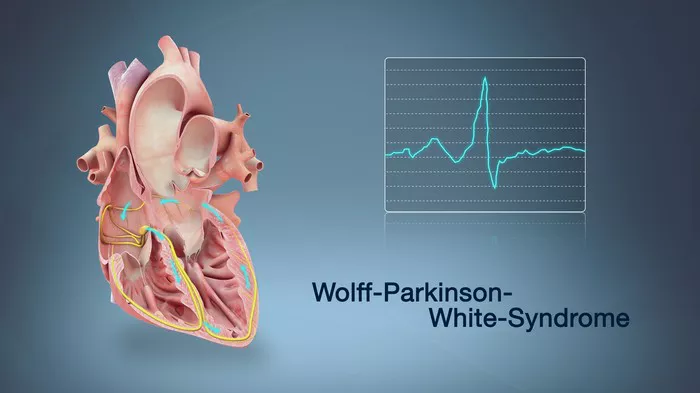
WPW is primarily caused by an extra electrical pathway in the heart, known as an accessory pathway, which connects the atria and ventricles. In a normal heart, electrical signals travel from the atria to the ventricles through the atrioventricular (AV) node, ensuring proper coordination of heartbeats. However, in individuals with WPW, the presence of an accessory pathway can lead to a condition called preexcitation.
Preexcitation occurs when electrical impulses bypass the AV node and travel directly from the atria to the ventricles through the accessory pathway. This can result in a rapid heartbeat, known as supraventricular tachycardia (SVT), which can be dangerous if left untreated. The exact cause of WPW is not always clear, but it is believed to be related to abnormal embryonic development of the heart’s electrical system.
Symptoms and Clinical Presentation
The symptoms of WPW can vary widely among individuals, with some experiencing no noticeable symptoms while others may have significant cardiac issues. Common symptoms associated with WPW include:
- Palpitations or rapid heartbeat
- Chest pain or discomfort
- Dizziness or lightheadedness
- Shortness of breath
- Fainting episodes (syncope)
- Fatigue or weakness
It is important to note that not everyone with WPW will experience symptoms, and the condition may only be discovered incidentally during routine medical exams or diagnostic tests.
Diagnosis and Evaluation
Diagnosing WPW typically involves a combination of clinical evaluation, electrocardiogram (ECG) recordings, and specialized cardiac tests. During an ECG, characteristic findings such as a shortened PR interval, widened QRS complex, and delta waves may indicate the presence of an accessory pathway and preexcitation.
Additional tests, such as Holter monitoring, exercise stress testing, and electrophysiology studies, may be performed to assess the severity of the condition, identify potential triggers for arrhythmias, and guide treatment decisions. Imaging studies such as echocardiography or cardiac MRI may also be utilized to evaluate the structure and function of the heart.
Complications and Risks
While WPW itself may not always cause symptoms or complications, certain factors can increase the risk of serious cardiac events in individuals with this condition. These include:
1. Atrial fibrillation (AFib): WPW patients are at higher risk of developing AFib, a chaotic and irregular heart rhythm that can lead to stroke, heart failure, and other complications if not managed properly.
2. Ventricular arrhythmias: In rare cases, WPW can predispose individuals to life-threatening ventricular arrhythmias such as ventricular fibrillation, which can result in sudden cardiac arrest.
3. Syncope and falls: Episodes of rapid heartbeat or fainting can increase the risk of falls and injuries, especially in older adults or those with underlying health conditions.
4. Cardiomyopathy: Chronic arrhythmias and abnormal heart rhythms can contribute to the development of cardiomyopathy, a condition characterized by weakened heart muscle and reduced cardiac function.
Management and Treatment Strategies
The management of WPW aims to control symptoms, prevent complications, and reduce the risk of arrhythmias and sudden cardiac events. Treatment strategies may include:
1. Medications: Antiarrhythmic drugs such as beta-blockers, calcium channel blockers, and antiarrhythmic agents may be prescribed to help regulate heart rhythm and prevent episodes of SVT or AFib.
2. Catheter ablation: Ablation therapy is a highly effective treatment for WPW, involving the use of catheters to deliver energy (radiofrequency or cryotherapy) to the accessory pathway, thereby disrupting its function and restoring normal electrical conduction.
3. Lifestyle modifications: Adopting a heart-healthy lifestyle with regular exercise, a balanced diet, smoking cessation, and stress management can help reduce the risk of arrhythmias and improve overall cardiovascular health.
4. Monitoring and follow-up: Regular cardiac monitoring, follow-up appointments with healthcare providers, and adherence to prescribed medications are essential components of long-term management for individuals with WPW.
Educating patients about their condition, potential triggers for arrhythmias, and the importance of adherence to treatment plans is crucial in empowering them to take an active role in managing their cardiac health.
Emergency Management and Prognosis
In emergency situations where WPW-related arrhythmias occur, prompt intervention is vital to stabilize the patient and prevent adverse outcomes. Basic life support (BLS) and advanced cardiac life support (ACLS) protocols should be followed, including cardioversion for unstable arrhythmias and medications such as adenosine or verapamil for acute SVT episodes.
The prognosis for individuals with WPW varies depending on several factors, including the presence of symptoms, the severity of arrhythmias, response to treatment, and overall cardiac health. With appropriate management and lifestyle modifications, many patients with WPW can lead fulfilling lives with minimal complications. However, close monitoring and ongoing care are essential to detect and address any changes or new developments in cardiac function.
Conclusion
In conclusion, Wolff-Parkinson-White Syndrome (WPW) is a potentially dangerous cardiac condition characterized by abnormal electrical pathways in the heart. While not everyone with WPW will experience symptoms or complications, the risk of serious arrhythmias and cardiac events underscores the importance of early diagnosis, appropriate management, and patient education. Healthcare providers play a critical role in evaluating and treating individuals with WPW, utilizing a multidisciplinary approach that encompasses clinical assessment, diagnostic testing, treatment interventions, and ongoing follow-up care. By raising awareness about WPW and its potential risks, we can work towards improving outcomes and enhancing the quality of life for affected individuals.