Left ventricular diastolic dysfunction is a condition that affects the ability of the heart’s left ventricle to relax and fill with blood properly during the diastolic phase of the cardiac cycle. This dysfunction can lead to various cardiovascular complications and is often associated with conditions such as hypertension, diabetes, and aging. In this article, we will delve into the causes of left ventricular diastolic dysfunction, its clinical significance, and potential treatment strategies.
An Overview of Left Ventricular Diastolic Dysfunction
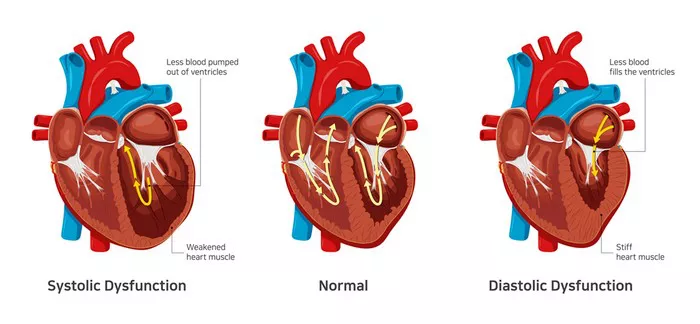
Before delving into the causes, let’s understand the normal functioning of the left ventricle during the cardiac cycle. During diastole, the heart relaxes, allowing blood to flow from the atria into the ventricles. The left ventricle then contracts during systole, pumping oxygen-rich blood to the rest of the body.
Left ventricular diastolic dysfunction occurs when the left ventricle stiffens, making it difficult for it to relax and fill adequately during diastole. This results in decreased cardiac output and can lead to symptoms such as shortness of breath, fatigue, and exercise intolerance. It is often seen in conjunction with left ventricular hypertrophy, a condition characterized by thickening of the ventricular walls due to chronic pressure overload.
Causes of Left Ventricular Diastolic Dysfunction
1. Hypertension: Chronic high blood pressure is one of the primary causes of left ventricular diastolic dysfunction. The increased pressure in the arteries forces the left ventricle to work harder to pump blood, leading to hypertrophy and stiffness of the ventricular walls over time.
2. Aging: As individuals age, the heart undergoes structural changes, including fibrosis and decreased compliance of the myocardium. These age-related changes contribute to left ventricular diastolic dysfunction, particularly in the elderly population.
3. Diabetes Mellitus: Uncontrolled diabetes can lead to the accumulation of advanced glycation end products (AGEs) in the myocardium, promoting fibrosis and stiffness of the left ventricle. Additionally, diabetes is often associated with other risk factors such as obesity and hypertension, further exacerbating diastolic dysfunction.
4. Obesity: Excess body weight and adipose tissue can contribute to systemic inflammation, insulin resistance, and metabolic abnormalities, all of which can impact cardiac function and contribute to left ventricular diastolic dysfunction.
5. Coronary Artery Disease (CAD): Atherosclerosis and coronary artery disease can impair myocardial perfusion, leading to myocardial ischemia and subsequent diastolic dysfunction. CAD is often seen in conjunction with other risk factors such as hypertension and diabetes.
6. Valvular Heart Disease: Conditions such as aortic stenosis or regurgitation can directly affect left ventricular function and contribute to diastolic dysfunction. The increased afterload or volume overload imposed by valvular abnormalities can lead to ventricular remodeling and stiffness.
7. Cardiomyopathies: Certain cardiomyopathies, such as hypertrophic cardiomyopathy or restrictive cardiomyopathy, can directly affect the compliance and relaxation of the left ventricle, leading to diastolic dysfunction.
8. Chronic Kidney Disease (CKD): CKD is associated with fluid overload, electrolyte imbalances, and uremic toxins that can contribute to cardiovascular complications, including left ventricular diastolic dysfunction.
9. Alcohol Consumption: Excessive alcohol intake can lead to cardiomyopathy and myocardial fibrosis, contributing to diastolic dysfunction. Alcohol-related cardiomyopathy is a well-recognized cause of heart failure with preserved ejection fraction (HFpEF).
10. Inflammatory Conditions: Chronic inflammatory conditions such as systemic lupus erythematosus (SLE) or rheumatoid arthritis (RA) can affect the myocardium and contribute to left ventricular diastolic dysfunction through mechanisms involving inflammation and autoimmune reactions.
Clinical Implications and Management
Left ventricular diastolic dysfunction is associated with an increased risk of heart failure, atrial fibrillation, and cardiovascular events. Diagnosis often involves echocardiography to assess ventricular function and measure parameters such as E/A ratio (early to late diastolic filling ratio), E/e’ ratio (ratio of early mitral inflow velocity to early diastolic mitral annular velocity), and deceleration time.
Management of left ventricular diastolic dysfunction focuses on addressing underlying causes and optimizing cardiovascular health. This may include lifestyle modifications such as weight management, blood pressure control, diabetes management, and limiting alcohol consumption. Pharmacological interventions such as angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, diuretics, and calcium channel blockers may be prescribed to improve symptoms and prevent progression.
Conclusion
Left ventricular diastolic dysfunction is a complex condition with multiple contributing factors. Understanding the underlying causes and implementing appropriate management strategies are essential in improving outcomes and reducing the risk of cardiovascular complications associated with this condition. Regular monitoring and collaboration between healthcare providers and patients are crucial in managing left ventricular diastolic dysfunction effectively.