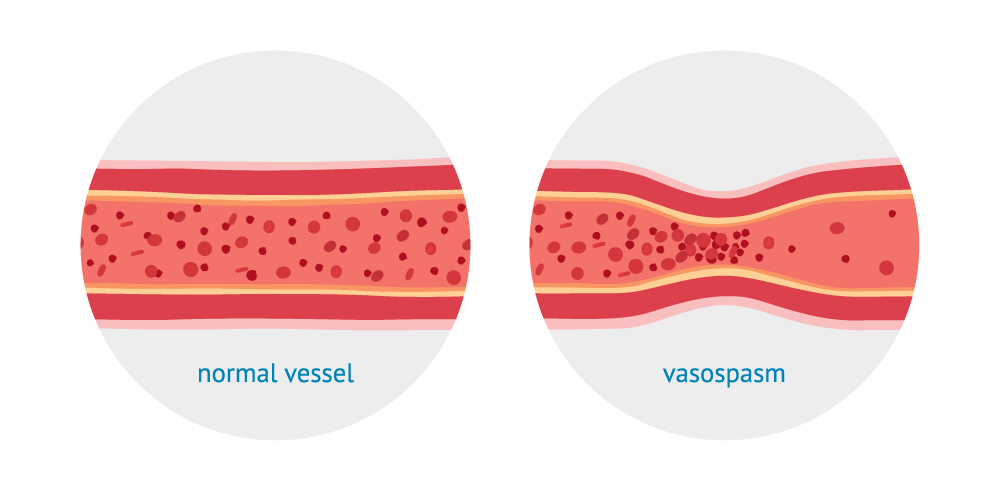
Vasospasm in the heart, also known as coronary artery vasospasm or variant angina, is a condition characterized by the sudden constriction or narrowing of coronary arteries, leading to reduced blood flow to the heart muscle. This phenomenon can result in angina (chest pain), heart attack, or even sudden cardiac death if not promptly treated. In this article, we will explore the causes and underlying mechanisms of vasospasm in the heart, shedding light on this critical aspect of cardiovascular health.
Coronary Artery Vasospasm: A Brief Overview
Before delving into the causes of vasospasm in the heart, it’s essential to understand the structure and function of coronary arteries. These arteries supply oxygen-rich blood to the heart muscle, ensuring its proper function. When these arteries experience sudden constriction or spasm, the flow of blood to the heart is disrupted, leading to potentially serious consequences.
Causes of Vasospasm in the Heart
1. Endothelial Dysfunction: One of the primary causes of vasospasm in the heart is endothelial dysfunction. The endothelium is the inner lining of blood vessels, including coronary arteries. When the endothelium becomes damaged or dysfunctional, it can lead to abnormal constriction and relaxation of the blood vessels, contributing to vasospasm.
2. Smooth Muscle Hyperreactivity: Another factor that can cause vasospasm in the heart is smooth muscle hyperreactivity. Smooth muscle cells line the walls of blood vessels, and when these cells become overly sensitive or hyperreactive, they can spasm and constrict, reducing blood flow through the arteries.
3. Neurogenic Factors: The nervous system plays a crucial role in regulating the tone of blood vessels, including coronary arteries. Neurogenic factors, such as increased sympathetic activity or abnormal nerve signaling, can trigger vasospasm by influencing the smooth muscle cells’ behavior in the blood vessel walls.
4. Hormonal Imbalances: Hormones also play a role in vascular function, and imbalances in hormone levels can contribute to vasospasm. For example, fluctuations in estrogen levels in women or hormonal imbalances in conditions like diabetes can affect blood vessel tone and contribute to vasospasm.
5. Drug-Induced Vasospasm: Certain medications, such as stimulants, vasoconstrictors, or drugs that affect the nervous system, can induce vasospasm in coronary arteries. It’s essential for healthcare providers to be aware of these potential side effects when prescribing medications to patients with cardiovascular conditions.
6. Environmental Triggers: External factors such as exposure to cold temperatures, emotional stress, or certain chemicals can trigger vasospasm in susceptible individuals. These triggers can activate pathways that lead to abnormal vascular responses and constriction of coronary arteries.
Mechanisms of Vasospasm in the Heart
Understanding the mechanisms underlying vasospasm in the heart can provide further insight into how this condition develops and progresses. Several key mechanisms contribute to the onset and perpetuation of vasospasm:
1. Calcium Ion Imbalance: Calcium ions play a crucial role in regulating smooth muscle contraction and relaxation. Dysregulation of calcium ion channels in smooth muscle cells can lead to excessive contraction and vasospasm in coronary arteries.
2. Endothelin Release: Endothelin is a potent vasoconstrictor produced by endothelial cells. Increased release of endothelin can promote vasoconstriction and contribute to vasospasm in the heart.
3. Nitric Oxide (NO) Deficiency: Nitric oxide is a vasodilator that helps regulate blood vessel tone. Reduced production or bioavailability of NO can lead to increased vascular tone and susceptibility to vasospasm.
4. Inflammatory Processes: Inflammation within the blood vessel walls can disrupt normal vascular function and contribute to vasospasm. Inflammatory mediators can promote smooth muscle contraction and vascular dysfunction.
5. Oxidative Stress: Excessive production of reactive oxygen species (ROS) can lead to oxidative stress, damaging blood vessel walls and promoting vasospasm. Antioxidant defenses play a critical role in protecting against oxidative damage and maintaining vascular health.
Clinical Implications and Management
Vasospasm in the heart has significant clinical implications, as it can lead to angina, myocardial infarction (heart attack), or even sudden cardiac death. Early recognition and management of vasospasm are essential to prevent adverse outcomes. Treatment strategies may include:
1. Nitrate Therapy: Nitroglycerin and other nitrates are commonly used to relieve vasospasm and improve blood flow to the heart.
2. Calcium Channel Blockers: Medications that block calcium channels can help relax blood vessels and prevent vasospasm.
3. Lifestyle Modifications: Avoiding triggers such as cold temperatures, stress, and certain medications can help reduce the risk of vasospasm recurrence.
4. Management of Underlying Conditions: Addressing underlying conditions such as hypertension, diabetes, and hyperlipidemia is crucial in managing vasospasm and reducing cardiovascular risk.
Conclusion
Vasospasm in the heart is a complex condition with multiple underlying causes and mechanisms. By understanding these factors, healthcare providers can effectively diagnose, treat, and manage vasospasm to improve patient outcomes and reduce the risk of cardiovascular events. Ongoing research into the pathophysiology of vasospasm is essential for developing new therapeutic strategies and enhancing our understanding of this critical aspect of heart health.