Supraventricular tachycardia (SVT) and ventricular tachycardia (VT) are two types of abnormal heart rhythms that can have serious implications for cardiovascular health. Understanding the differences between SVT and VT, as well as their respective risks and management strategies, is crucial for healthcare professionals and patients alike. In this article, we will delve into the complexities of SVT and VT, explore their potential dangers, and discuss how they are diagnosed and treated.
Understanding Supraventricular Tachycardia (SVT)
SVT is a rapid heart rhythm originating from above the ventricles, typically in the atria or atrioventricular node. It is characterized by a fast and regular heartbeat, often exceeding 100 beats per minute. SVT can occur in individuals with structurally normal hearts or those with underlying heart conditions such as coronary artery disease, congenital heart defects, or electrolyte imbalances.
Risk Factors and Symptoms of SVT
Several factors can contribute to the development of SVT, including:
1. Genetics: A family history of arrhythmias may increase the risk of SVT.
2. Stress and Anxiety: Emotional triggers can lead to episodes of SVT.
3. Stimulant Use: Caffeine, nicotine, and certain medications can provoke SVT.
4. Hormonal Changes: Pregnancy or thyroid disorders may predispose individuals to SVT.
Common symptoms of SVT include palpitations, rapid heartbeat, chest discomfort, dizziness, lightheadedness, and fainting. In some cases, SVT episodes may resolve spontaneously, but persistent or recurrent episodes require medical evaluation and management.
Diagnosis of SVT
The diagnosis of SVT involves a comprehensive assessment that may include:
1. Medical History: Gathering information about symptoms, triggers, and past medical conditions.
2. Physical Examination: Checking vital signs, heart sounds, and signs of heart failure.
3. Electrocardiogram (ECG): Recording the heart’s electrical activity during an SVT episode.
4. Holter Monitor: Continuous ECG monitoring over 24-48 hours to capture intermittent SVT episodes.
5. Electrophysiology Study (EPS): Invasive procedure to map and identify the site of SVT origin.
Treatment Strategies for SVT
The management of SVT aims to control symptoms, prevent recurrence, and reduce the risk of complications. Treatment options may include:
1. Vagal Maneuvers: Non-invasive techniques such as bearing down or cold water immersion.
2. Medications: Beta-blockers, calcium channel blockers, and antiarrhythmic drugs to slow heart rate and restore normal rhythm.
3. Cardioversion: Electrical shock to reset the heart’s rhythm in acute SVT episodes.
4. Catheter Ablation: Minimally invasive procedure to destroy abnormal heart tissue causing SVT.
Understanding Ventricular Tachycardia (VT)
VT is a rapid heart rhythm originating from the ventricles, the lower chambers of the heart responsible for pumping blood to the body. Unlike SVT, VT is often associated with structural heart abnormalities such as prior heart attacks, cardiomyopathy, or scar tissue from surgeries.
Risk Factors and Symptoms of VT
The risk factors for VT include:
1. Coronary Artery Disease: Narrowed or blocked arteries can lead to ischemic VT.
2. Heart Failure: Impaired heart function increases the risk of VT.
3. Cardiomyopathy: Enlarged or weakened heart muscle predisposes to VT.
4. Electrolyte Imbalances: Abnormal levels of potassium, magnesium, or calcium can trigger VT.
Symptoms of VT may vary depending on its duration and severity but can include palpitations, chest pain, shortness of breath, dizziness, fainting, and cardiac arrest in severe cases.
Diagnosis of VT
The diagnosis of VT involves similar assessments as SVT, including:
1. Medical History: Identifying underlying heart conditions and potential triggers.
2. Physical Examination: Evaluating cardiac signs and symptoms.
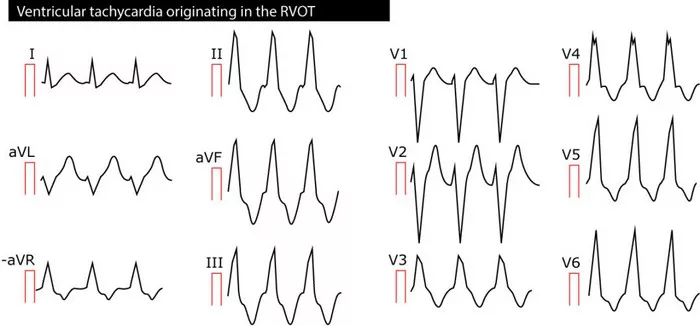
3. Electrocardiogram (ECG): Characteristic ECG patterns indicating ventricular origin of tachycardia.
4. Holter Monitor: Continuous ECG monitoring to detect intermittent VT episodes.
5. Echocardiogram: Imaging to assess heart structure and function.
Treatment Strategies for VT
The management of VT depends on its severity and associated risks. Treatment options may include:
1. Medications: Antiarrhythmic drugs to stabilize heart rhythm and prevent recurrence.
2. Implantable Cardioverter-Defibrillator (ICD): Device implantation to deliver shocks and restore normal rhythm during VT episodes.
3. Catheter Ablation: Targeted destruction of abnormal heart tissue causing VT.
4. Cardioversion: Electrical shock to terminate sustained VT episodes.
Comparing the Risks of SVT and VT
While both SVT and VT can be concerning arrhythmias, VT is generally considered more dangerous due to its association with structural heart disease and the potential for life-threatening complications such as ventricular fibrillation and sudden cardiac arrest. VT episodes can result in hemodynamic instability, decreased cardiac output, and even death if not promptly treated.
SVT, although less likely to cause immediate life-threatening events, can still lead to significant symptoms, impair quality of life, and require medical intervention to prevent complications such as heart failure or stroke.
Conclusion
In conclusion, both SVT and VT are abnormal heart rhythms that require careful evaluation, diagnosis, and management. While SVT is characterized by rapid heartbeats originating above the ventricles and is often manageable with medications or procedures like catheter ablation, VT originating in the ventricles is more concerning due to its association with structural heart abnormalities and the potential for serious complications. Early recognition, appropriate treatment, and regular follow-up are essential in reducing the risks associated with SVT and VT, improving patient outcomes, and enhancing overall cardiovascular health.