In the wake of the COVID-19 pandemic, mRNA vaccines have been heralded as a monumental stride in medical science, offering robust protection against a virus that has claimed millions of lives worldwide. Developed at an unprecedented pace, these vaccines have been instrumental in curbing the spread of the disease and reducing the severity of its outcomes. However, amidst their widespread use and success, reports of myocarditis — inflammation of the heart muscle — following vaccination have emerged, prompting a closer examination of this phenomenon. This article delves into the underlying mechanisms, the incidence rates, and the implications of myocarditis associated with mRNA vaccines, aiming to provide a comprehensive understanding of why this condition occurs and how it impacts the vaccinated population.
The Mechanism of mRNA Vaccines
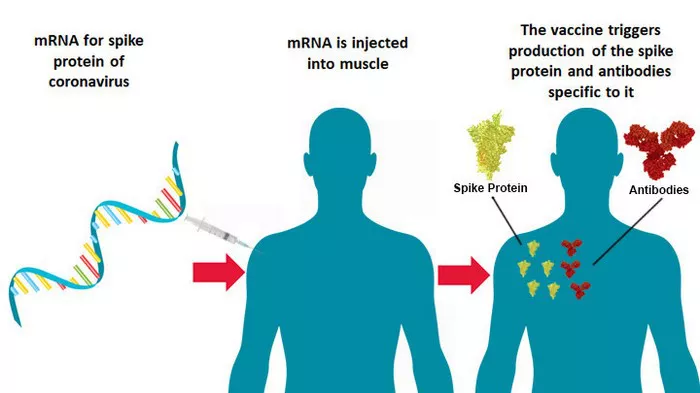
To appreciate the context of myocarditis cases, it’s essential to understand how mRNA vaccines work. mRNA (messenger RNA) vaccines utilize a snippet of the virus’s genetic code to instruct cells in the body to produce a protein unique to the virus, in this case, the spike protein of SARS-CoV-2. This process does not involve the virus itself, nor does it alter human DNA. Instead, it prompts an immune response, preparing the body to recognize and combat the virus if exposed in the future.
Incidence of Myocarditis Following mRNA Vaccination
Myocarditis following mRNA vaccination has been reported, albeit at a low rate. According to data from various health organizations worldwide, these instances are rare when compared to the millions of vaccine doses administered. Notably, the condition has been observed more frequently in younger male populations, typically following the second dose of the vaccine.
Delving into the Causes
The precise mechanisms through which mRNA vaccines might lead to myocarditis remain the subject of ongoing research. However, several hypotheses have been proposed to explain this phenomenon:
1. Immune Response Hypothesis: The most widely accepted theory suggests that myocarditis may arise from an overactive immune response to the vaccine. In some individuals, the immune system’s reaction to the spike protein produced following vaccination may inadvertently target similar proteins present in heart muscle cells, leading to inflammation.
2. Molecular Mimicry: Another theory is based on molecular mimicry, where certain sequences in the spike protein might closely resemble those in heart muscle cells. This similarity could lead to an autoimmune response, where the body attacks its own cells, mistaking them for foreign invaders.
3. Adjuvant Effect: Some researchers propose that the vaccine’s lipid nanoparticles — which encapsulate the mRNA to ensure its delivery into cells — may act as an adjuvant, enhancing the immune response to an extent that could contribute to heart muscle inflammation in susceptible individuals.
Risk Factors and Epidemiology
Identifying the risk factors for developing myocarditis after an mRNA vaccine is crucial for understanding its epidemiology. Age, sex, and possibly underlying health conditions seem to play a role. The highest incidence has been observed in males aged 16 to 29 years. The reasons behind this demographic susceptibility are not entirely clear but may involve hormonal differences, variations in immune system responses, or genetic predispositions.
Clinical Presentation and Outcomes
Patients with vaccine-related myocarditis typically present with chest pain, shortness of breath, or palpitations within a week after receiving the vaccine. Fortunately, the majority of cases have been mild, with patients recovering fully with standard treatment for myocarditis, such as anti-inflammatory medications and monitoring for potential complications. Severe outcomes have been exceedingly rare.
Comparative Risks: Vaccination vs. Infection
When considering the risk of myocarditis, it’s imperative to compare the incidence following vaccination to that associated with COVID-19 infection. Research consistently shows that the risk of myocarditis is significantly higher following infection than vaccination. Moreover, COVID-19 infection can lead to a broader range of severe cardiac complications, underscoring the protective benefits of vaccination.
Addressing Public Concerns
The occurrence of myocarditis post-mRNA vaccination has raised public concern, potentially influencing vaccine hesitancy. Addressing these concerns transparently is critical. Health authorities and researchers have been diligent in monitoring, reporting, and investigating these cases, emphasizing that the benefits of vaccination overwhelmingly outweigh the risks. Public health communications have focused on educating the public about the rarity of myocarditis, the availability of treatment, and the comparative risks of COVID-19 infection.
Future Directions in Research and Vaccine Development
Ongoing and future research aims to elucidate the mechanisms behind vaccine-associated myocarditis, identify potential risk factors, and develop strategies to mitigate this side effect. This includes the exploration of vaccine dosing intervals, formulations, and targeted advice for populations at higher risk. Moreover, as vaccine technology evolves, next-generation vaccines may further minimize the risk of adverse effects while maintaining efficacy against the virus.
Conclusion
The development and deployment of mRNA vaccines represent a significant achievement in the fight against COVID-19. While the association with myocarditis warrants attention and ongoing research, the incidence of this condition isAC rare, especially when weighed against the risks posed by the virus itself. Understanding and communicating the balance of risks and benefits is paramount to sustaining public trust and vaccine uptake. As science advances, continued vigilance, research, and adaptation of vaccine strategies will be essential in mitigating risks and protecting public health in the face of emerging infectious threats.