The human body is a marvel of complexity, with intricate systems working in harmony to maintain optimal health. One such system is the autonomic nervous system (ANS), responsible for regulating vital functions like heart rate, digestion, and blood pressure. Within the ANS, the vagus nerve plays a crucial role, and its interaction with blood pressure regulation is of particular interest. In this article, we will explore the anatomy and function of the vagus nerve, how it can trigger sudden drops in blood pressure, and the implications of this phenomenon for medical science.
Anatomy of the Vagus Nerve
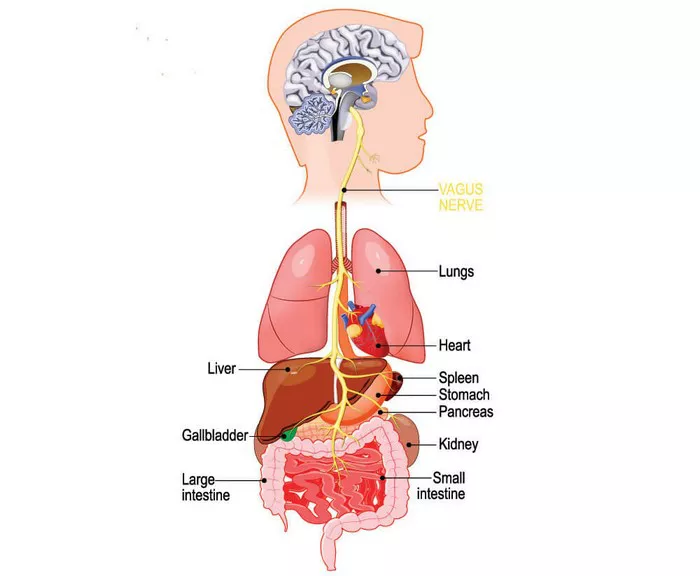
The vagus nerve, also known as cranial nerve X, is the longest cranial nerve in the body, extending from the brainstem to multiple organs in the chest and abdomen. It is a mixed nerve, meaning it contains both sensory and motor fibers, and it plays a vital role in parasympathetic nervous system function.
The vagus nerve emerges from the medulla oblongata, a part of the brainstem, and travels down through the neck, where it branches out extensively to innervate various organs. These organs include the heart, lungs, stomach, and intestines, among others. This widespread connectivity allows the vagus nerve to influence numerous physiological processes throughout the body.
Function of the Vagus Nerve
The primary function of the vagus nerve is to regulate the parasympathetic nervous system, which is responsible for the body’s “rest and digest” response. This stands in contrast to the sympathetic nervous system, which triggers the “fight or flight” response. The vagus nerve helps maintain homeostasis by promoting activities that conserve energy and facilitate recovery after periods of stress or exertion.
Some key functions of the vagus nerve include:
1. Heart Rate Regulation: The vagus nerve exerts a significant influence on heart rate by slowing it down. This effect is particularly notable during periods of relaxation or low activity when the parasympathetic system is dominant.
2. Respiratory Control: The vagus nerve plays a role in regulating breathing patterns, ensuring that oxygen intake and carbon dioxide elimination remain within optimal ranges.
3. Digestive Function: Through its branches that reach the digestive organs, the vagus nerve helps stimulate digestive juices, regulate gut motility, and promote nutrient absorption.
4. Blood Pressure Regulation: The vagus nerve contributes to blood pressure regulation by influencing blood vessel dilation and constriction, as well as by modulating heart rate, which indirectly affects blood pressure.
The Baroreceptor Reflex and Blood Pressure Regulation
One of the key mechanisms through which the body maintains stable blood pressure is the baroreceptor reflex. Baroreceptors are specialized sensory receptors located in the walls of certain blood vessels, particularly in the carotid sinuses (found in the neck) and the aortic arch (located near the heart). These receptors continuously monitor blood pressure and send signals to the brainstem, specifically the medulla oblongata, in response to changes in pressure.
When blood pressure rises, baroreceptors detect the increase and send inhibitory signals via the vagus nerve and other nerves to the cardiovascular center in the medulla oblongata. This leads to a decrease in sympathetic activity and an increase in parasympathetic activity. As a result, heart rate decreases, blood vessels dilate, and blood pressure normalizes.
Conversely, when blood pressure drops, such as during sudden changes in posture or dehydration, baroreceptors detect the decrease and send stimulatory signals to the cardiovascular center. This results in increased sympathetic activity, causing the heart to beat faster, blood vessels to constrict, and blood pressure to rise back to a healthier level.
The Role of the Vagus Nerve in Sudden Drops in Blood Pressure
While the vagus nerve is primarily associated with promoting relaxation and lowering heart rate, it can also play a role in causing sudden drops in blood pressure under certain conditions. This phenomenon is known as vasovagal syncope, and it occurs when the vagus nerve is overstimulated, leading to a rapid decrease in blood pressure and temporary loss of consciousness.
Vasovagal syncope can be triggered by various factors, including:
1. Emotional Stress: Intense emotional experiences, such as fear, anxiety, or emotional trauma, can activate the vagus nerve and trigger a vasovagal response. This is why some individuals may faint during highly stressful situations.
2. Pain or Discomfort: Severe pain or discomfort, such as from a medical procedure or injury, can stimulate the vagus nerve and cause a sudden drop in blood pressure. This is sometimes observed in individuals with a low pain threshold or certain medical conditions.
3. Prolonged Standing: Remaining in an upright position for an extended period, especially in hot environments, can lead to blood pooling in the legs and reduced venous return to the heart. This can activate the vagus nerve and contribute to orthostatic hypotension, a form of low blood pressure upon standing.
4. Dehydration or Volume Loss: Inadequate fluid intake, excessive sweating, vomiting, or diarrhea can lead to dehydration and reduced blood volume. This, in turn, can trigger a vasovagal response as the body attempts to maintain blood pressure.
5. Certain Medications: Some medications, such as blood pressure-lowering drugs, diuretics, or medications that affect the autonomic nervous system, can increase the risk of vasovagal syncope by altering vascular tone or heart rate control.
Clinical Implications and Management
Vasovagal syncope is a common cause of fainting episodes and is typically benign, meaning it does not indicate a serious underlying medical condition. However, recurrent episodes of syncope can significantly impact an individual’s quality of life and may warrant medical evaluation and management.
In clinical practice, the management of vasovagal syncope often involves:
1. Identifying Triggers: Healthcare providers work with patients to identify specific triggers that may lead to vasovagal episodes. This may involve keeping a symptom diary or undergoing specialized testing, such as tilt table testing, to provoke and evaluate fainting responses.
2. Lifestyle Modifications: Making lifestyle changes, such as staying well-hydrated, avoiding prolonged standing or extreme heat, and managing stress through relaxation techniques or therapy, can help reduce the frequency of vasovagal episodes.
3. Medication: In some cases, medications that increase blood volume (such as fludrocortisone) or that target heart rate and blood pressure regulation (such as beta-blockers) may be prescribed to prevent syncope episodes. However, the use of medications requires careful consideration of potential side effects and individual response.
4. Physical Counterpressure Maneuvers: Techniques like leg crossing and muscle tensing (applied tension) can help counteract vasovagal responses by promoting venous return to the heart and maintaining blood pressure.
5. Implantable Devices: For individuals with severe and refractory vasovagal syncope, implantable devices such as pacemakers or loop recorders may be considered. These devices can monitor heart rhythm and provide therapeutic interventions if abnormal rhythms or pauses are detected.
Conclusion
The vagus nerve plays a multifaceted role in regulating various bodily functions, including blood pressure control. While it is primarily associated with promoting relaxation and parasympathetic activity, overstimulation of the vagus nerve can lead to sudden drops in blood pressure, as seen in vasovagal syncope. Understanding the mechanisms underlying vasovagal syncope is crucial for healthcare providers to effectively manage and support individuals experiencing fainting episodes.
As research continues to unravel the complexities of the autonomic nervous system and its interactions with blood pressure regulation, new insights into the diagnosis and treatment of vasovagal syncope may emerge. Advances in technology, such as wearable devices for continuous monitoring and non-invasive interventions, offer promising avenues for improving patient outcomes and quality of life.
In conclusion, the vagus nerve’s ability to trigger sudden drops in blood pressure highlights the intricate balance within the autonomic nervous system and underscores the importance of comprehensive assessment and personalized management strategies for individuals prone to vasovagal syncope. By integrating clinical expertise with scientific advancements, healthcare providers can better support patients in navigating and mitigating the challenges associated with autonomic dysfunction and syncope disorders.