Irbesartan is a widely prescribed medication used to manage hypertension (high blood pressure) and certain kidney conditions related to diabetes. As with many medications, the timing of irbesartan intake can significantly impact its effectiveness and potential side effects. Understanding the best time to take irbesartan is crucial for optimizing its therapeutic benefits and ensuring patient well-being. In this article, we delve into the pharmacokinetics of irbesartan, explore the factors influencing its timing, discuss existing research, and provide practical recommendations for patients and healthcare providers.
Pharmacokinetics of Irbesartan
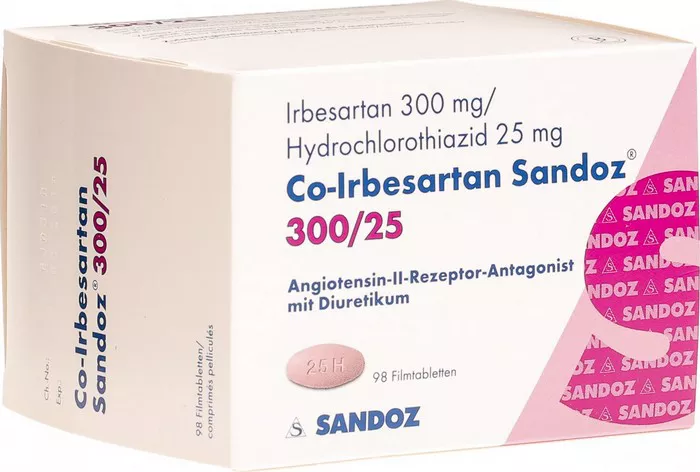
Before delving into the best time to take irbesartan, it’s essential to understand its pharmacokinetics—the study of how drugs move through the body. Irbesartan is an angiotensin II receptor blocker (ARB) that works by blocking the action of angiotensin II, a hormone that constricts blood vessels, thereby lowering blood pressure and improving blood flow.
Upon oral administration, irbesartan is rapidly absorbed from the gastrointestinal tract, reaching peak plasma concentrations within 1 to 2 hours. The drug undergoes minimal first-pass metabolism in the liver and has a bioavailability of approximately 60-80%. Irbesartan is primarily eliminated via hepatic metabolism and biliary excretion, with a half-life of around 11-15 hours in healthy individuals. These pharmacokinetic properties lay the groundwork for determining the optimal timing of irbesartan administration.
Factors Influencing Irbesartan Timing
Several factors can influence the timing of irbesartan intake and its efficacy:
1. Blood Pressure Control: Irbesartan’s primary indication is the management of hypertension. Given that blood pressure typically follows a circadian rhythm, with higher readings in the morning, taking irbesartan in the morning may align with the body’s natural mechanisms for blood pressure control.
2. Diurnal Variation of Cardiovascular Events: Research suggests that cardiovascular events such as heart attacks and strokes often occur more frequently in the morning. Therefore, taking medications like irbesartan in the morning may provide enhanced protection during this critical period.
3. Adverse Effects: Irbesartan, like other ARBs, can cause side effects such as dizziness and fatigue. Timing the medication to coincide with periods of low activity or before bedtime may help mitigate these side effects.
4. Compliance and Convenience: Consideration of patients’ daily routines and habits is crucial to ensure adherence to medication regimens. Choosing a time that aligns with a patient’s lifestyle can improve compliance and treatment outcomes.
Existing Research on Irbesartan Timing
Numerous studies have explored the optimal timing of irbesartan administration. While some research suggests that taking irbesartan in the morning may be more effective in lowering blood pressure, other studies have not found significant differences between morning and evening dosing. Let’s examine some key findings:
1. Morning vs. Evening Dosing: A study published in the Journal of Human Hypertension compared the effects of morning versus evening dosing of irbesartan in patients with hypertension. The researchers found that both morning and evening dosing resulted in similar reductions in blood pressure, indicating that the timing of irbesartan intake may not significantly impact its efficacy.
2. Chronotherapy: Chronotherapy involves timing medications based on the body’s circadian rhythms to optimize treatment outcomes. While some studies have explored chronotherapy with other antihypertensive medications, such as calcium channel blockers, limited research specifically focuses on chronotherapy with irbesartan.
3. Patient-Specific Factors: Individual variations in circadian rhythms, lifestyle factors, and comorbidities can influence the optimal timing of irbesartan for each patient. Personalized medicine approaches may be beneficial in tailoring treatment strategies based on these factors.
Practical Recommendations
Based on the available evidence and clinical experience, the following practical recommendations can guide the optimal timing of irbesartan administration:
1. Consistency: Irbesartan should be taken at the same time each day to maintain steady drug levels in the body and maximize therapeutic effects.
2. Morning vs. Evening Dosing: While there is no definitive consensus on whether morning or evening dosing is superior, patients can discuss their preferences and lifestyle factors with healthcare providers to determine the most suitable timing.
3. Consider Individual Factors: Healthcare providers should consider individual patient factors, such as blood pressure patterns, comorbidities, medication adherence, and potential side effects, when recommending the timing of irbesartan intake.
4. Monitoring and Adjustment: Regular monitoring of blood pressure and clinical response to irbesartan is essential. Adjustments to the timing or dosage of irbesartan may be necessary based on individual patient needs and treatment goals.
Conclusion
Optimizing the timing of irbesartan administration is a multifaceted process that involves understanding its pharmacokinetics, considering patient-specific factors, and evaluating existing research. While there is no one-size-fits-all approach to timing irbesartan intake, healthcare providers can collaborate with patients to develop individualized treatment plans that maximize efficacy, minimize side effects, and improve overall patient outcomes. By incorporating evidence-based practices and personalized medicine principles, we can enhance the therapeutic benefits of irbesartan in managing hypertension and related conditions.