Myocarditis, an inflammatory condition affecting the heart muscle, presents a diagnostic challenge due to its diverse clinical manifestations and variable disease course. Electrocardiography (EKG or ECG) is a commonly used diagnostic tool in the evaluation of patients with suspected myocarditis, providing valuable information about cardiac electrical activity and potential myocardial abnormalities. However, the utility of EKG in diagnosing myocarditis is limited by its nonspecific findings and inability to definitively confirm the presence of myocardial inflammation.
Introduction to Myocarditis And Electrocardiography:
Myocarditis is characterized by inflammation of the heart muscle, which can result from various infectious, autoimmune, toxic, or hypersensitivity etiologies. The clinical presentation of myocarditis can vary widely, ranging from asymptomatic cases to life-threatening complications such as heart failure, arrhythmias, or sudden cardiac death. Electrocardiography is a valuable diagnostic tool in the evaluation of patients with suspected myocarditis, allowing for the assessment of cardiac electrical activity and identification of potential myocardial abnormalities.
Common EKG Findings in Myocarditis:
While EKG findings in myocarditis can be variable and nonspecific, several characteristic abnormalities may be observed, including:
ST-segment and T-wave changes: Myocarditis may present with ST-segment elevation or depression, T-wave inversion, or nonspecific ST-T wave abnormalities on EKG. These changes may be indicative of myocardial ischemia, injury, or inflammation and can occur in a diffuse or focal distribution.
Arrhythmias: Myocarditis can predispose individuals to various arrhythmias, including atrial fibrillation, atrial flutter, ventricular ectopy, ventricular tachycardia, or heart block. Arrhythmias may manifest as irregular heart rhythms, widened QRS complexes, prolonged QT intervals, or conduction delays on EKG.
Sinus tachycardia: Sinus tachycardia, characterized by an elevated heart rate (>100 beats per minute) with normal sinus rhythm, may be observed in patients with myocarditis due to sympathetic activation, fever, or hemodynamic instability.
Low voltage: Myocarditis-associated myocardial inflammation and edema may lead to decreased QRS voltage on EKG, characterized by reduced amplitude of QRS complexes in multiple leads.
Limitations of EKG in Myocarditis Diagnosis:
Despite its utility, EKG has several limitations in the diagnosis of myocarditis, including:
Nonspecific findings: EKG findings in myocarditis are often nonspecific and can overlap with those of other cardiac or noncardiac conditions.
Temporal variability: EKG findings in myocarditis may be transient and dynamic, evolving over time as the inflammatory process progresses or resolves. Serial EKG monitoring may be necessary to detect changes in cardiac electrical activity and assess treatment response in patients with myocarditis.
Limited sensitivity and specificity: EKG has limited sensitivity and specificity for detecting myocardial inflammation or diagnosing myocarditis. Normal EKG findings do not exclude the presence of myocarditis, particularly in patients with subclinical or mild disease. Conversely, abnormal EKG findings may be nonspecific and require further evaluation to confirm the diagnosis of myocarditis and identify potential complications.
Role of EKG in Myocarditis Evaluation:
Despite its limitations, EKG remains a valuable diagnostic tool in the evaluation of patients with suspected myocarditis, providing important clinical information about cardiac electrical activity and potential myocardial abnormalities. EKG findings may raise suspicion for myocarditis and guide further diagnostic workup, including laboratory tests, imaging studies, and endomyocardial biopsy. Additionally, EKG monitoring may help assess the severity of myocardial involvement, guide treatment decisions, and monitor for arrhythmias or conduction disturbances in patients with myocarditis.
Integration of EKG with Other Diagnostic Modalities:
In the evaluation of myocarditis, EKG findings should be interpreted in conjunction with other diagnostic modalities to establish a comprehensive assessment of cardiac structure, function, and inflammation.
Additional tests commonly used in the evaluation of myocarditis include:
Cardiac biomarkers: Measurement of cardiac biomarkers such as troponin and creatine kinase-MB (CK-MB) can help assess myocardial injury and inflammation in patients with suspected myocarditis.
Echocardiography: Transthoracic echocardiography (TTE) allows for the assessment of cardiac structure and function, detection of regional wall motion abnormalities, and identification of pericardial effusion or other cardiac abnormalities suggestive of myocarditis.
Cardiac MRI: Cardiac magnetic resonance imaging (MRI) is considered the gold standard for noninvasive diagnosis of myocarditis, providing detailed assessment of myocardial inflammation, edema, fibrosis, and perfusion defects.
Endomyocardial biopsy: In select cases, endomyocardial biopsy may be performed to confirm the presence of myocardial inflammation and characterize the underlying etiology of myocarditis.
Conclusion:
In conclusion, electrocardiography plays a valuable role in the evaluation of patients with suspected myocarditis, providing important clinical information about cardiac electrical activity and potential myocardial abnormalities. While EKG findings in myocarditis can be nonspecific and require correlation with clinical context and additional diagnostic studies, they can raise suspicion for myocardial inflammation and guide further evaluation and management.
Integration of EKG with other diagnostic modalities, including cardiac biomarkers, echocardiography, cardiac MRI, and endomyocardial biopsy, allows for a comprehensive assessment of myocarditis and optimization of patient care and outcomes.
FAQs
Can an electrocardiogram detect myocardial infarction?
Yes, an electrocardiogram (EKG or ECG) is a valuable tool for detecting myocardial infarction (MI), commonly known as a heart attack. During an MI, there is inadequate blood flow to a portion of the heart muscle, leading to myocardial ischemia and injury. The EKG may show characteristic changes indicative of myocardial infarction, including:
ST-segment elevation (STEMI): Elevation of the ST segment in specific leads indicates acute transmural myocardial ischemia and is characteristic of STEMI (ST-segment elevation myocardial infarction).
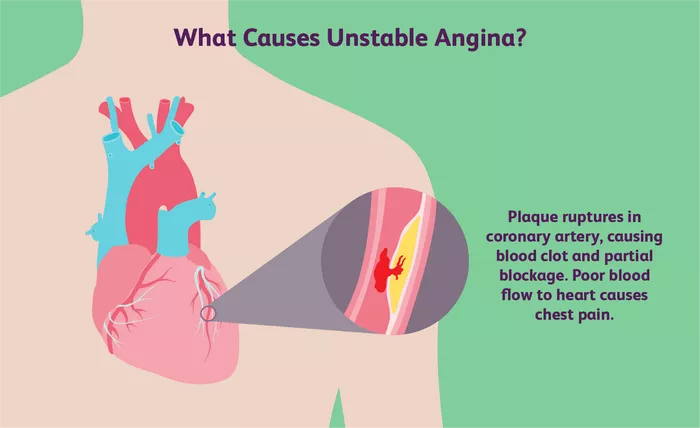
ST-segment depression or T-wave inversion: These changes may indicate subendocardial ischemia and are seen in non-ST elevation myocardial infarction (NSTEMI) or unstable angina.
Pathological Q waves: Development of Q waves in specific leads may suggest previous myocardial necrosis and is a marker of prior MI.
What diseases can be detected by electrocardiogram?
Electrocardiography is a versatile diagnostic tool used to detect various cardiac conditions, including:
Arrhythmias: EKG can identify abnormalities in heart rhythm, including atrial fibrillation, atrial flutter, supraventricular tachycardia, ventricular tachycardia, and bradyarrhythmias.
Myocardial ischemia and infarction: Changes in ST segments, T waves, and Q waves on EKG may indicate myocardial ischemia or infarction.
Conduction abnormalities: EKG can detect conduction disturbances such as bundle branch blocks, atrioventricular blocks, and intraventricular conduction delays.
Cardiac hypertrophy: EKG findings may suggest left ventricular hypertrophy, right ventricular hypertrophy, or biatrial enlargement.
Pericardial disease: EKG may show characteristic changes in pericarditis, including diffuse ST-segment elevation and PR-segment depression (saddle-shaped ST elevation).
How to judge whether it is myocarditis?
Judging whether a patient has myocarditis involves a comprehensive approach that considers clinical history, symptoms, physical examination findings, laboratory tests, imaging studies, and diagnostic procedures. Key steps in the evaluation of suspected myocarditis include:
Clinical assessment: Evaluate for symptoms suggestive of myocarditis, such as chest pain, shortness of breath, fatigue, palpitations, or signs of heart failure.
Laboratory tests: Measure cardiac biomarkers (troponin, creatine kinase) to assess for myocardial injury, as well as inflammatory markers (C-reactive protein, erythrocyte sedimentation rate) to evaluate for systemic inflammation.
Electrocardiography: Perform an EKG to assess for characteristic changes suggestive of myocarditis, such as ST-segment and T-wave abnormalities, arrhythmias, or conduction disturbances.
Imaging studies: Obtain transthoracic echocardiography (TTE) to assess cardiac structure and function, detect regional wall motion abnormalities, and identify pericardial effusion or other abnormalities suggestive of myocarditis.