Living with 20% heart function, often referred to as a severely reduced ejection fraction, is a serious and life-altering condition that requires careful management and medical intervention. The ejection fraction (EF) measures the percentage of blood pumped out of the heart’s left ventricle with each contraction. A normal EF ranges from 55% to 70%, while an EF below 40% is considered reduced, and an EF of 20% signifies severe heart failure. This article will explore the prognosis, management strategies, lifestyle adjustments, and potential treatments for individuals living with such a low EF.
Understanding Ejection Fraction And Heart Function
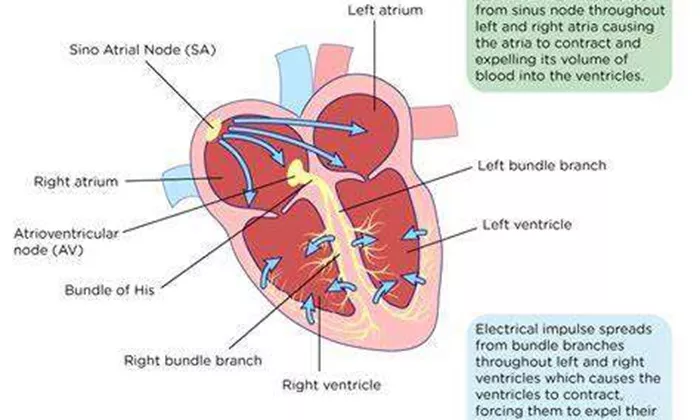
Ejection fraction is a key indicator of heart health, reflecting the heart’s efficiency in pumping blood. When the EF drops to 20%, the heart’s ability to supply the body with oxygen-rich blood is significantly compromised. This can lead to symptoms such as shortness of breath, fatigue, swelling in the legs and abdomen, and difficulty performing everyday activities. The underlying causes of a reduced EF can vary, including conditions like coronary artery disease, myocardial infarction (heart attack), cardiomyopathy, and chronic hypertension.
Prognosis And Life Expectancy with 20% Heart Function
The prognosis for individuals with a severely reduced EF depends on several factors, including the underlying cause of heart failure, the patient’s overall health, comorbid conditions, and adherence to treatment. It is challenging to provide a precise life expectancy for someone with an EF of 20%, as it can vary widely from person to person.
However, studies and clinical data suggest that the average life expectancy for individuals with severe heart failure and a low EF can range from a few months to several years. Some patients may live longer with proper medical management, lifestyle changes, and advanced treatments, while others may experience a more rapid decline.
Medical Management And Treatment Options
Effective management of heart failure with a low EF involves a combination of medications, lifestyle modifications, and sometimes surgical interventions. The primary goals of treatment are to improve symptoms, enhance quality of life, and prevent further deterioration of heart function. Key treatment strategies include:
Medications
ACE Inhibitors and ARBs: These medications help relax blood vessels, lower blood pressure, and reduce the heart’s workload.
Beta-Blockers: These drugs slow the heart rate, reduce blood pressure, and improve heart function.
Diuretics: Often referred to as “water pills,” diuretics help reduce fluid buildup in the body, easing symptoms like swelling and shortness of breath.
Aldosterone Antagonists: These medications help manage fluid retention and reduce the risk of hospitalization.
Inotropes: In cases of severe heart failure, inotropic agents may be used to increase the strength of heart contractions.
Lifestyle Modifications
Dietary Changes: A heart-healthy diet low in sodium, saturated fats, and cholesterol can help manage symptoms and improve overall health.
Regular Exercise: While strenuous activity may not be advisable, moderate exercise under medical supervision can improve heart function and quality of life.
Smoking Cessation: Quitting smoking is crucial for heart health and can significantly improve outcomes.
Weight Management: Maintaining a healthy weight reduces the heart’s workload and improves overall health.
Surgical Interventions and Advanced Treatments
Implantable Cardioverter-Defibrillators (ICDs): These devices monitor heart rhythms and deliver shocks to correct potentially life-threatening arrhythmias.
Cardiac Resynchronization Therapy (CRT): CRT devices help coordinate the contractions of the heart’s ventricles, improving efficiency and symptoms.
Left Ventricular Assist Devices (LVADs): LVADs are mechanical pumps that assist the heart in pumping blood, often used as a bridge to heart transplantation or as long-term therapy.
Heart Transplant: For eligible patients with end-stage heart failure, a heart transplant may be the best option to significantly extend life expectancy and improve quality of life.
Living with 20% Heart Function: Daily Life And Coping Strategies
Adjusting to life with severe heart failure requires significant changes and a proactive approach to health management.
Here are some tips and strategies to help individuals cope with their condition:
Monitoring Symptoms and Health
Regular monitoring of symptoms and vital signs, such as weight, blood pressure, and heart rate, can help detect early signs of worsening heart failure. Keeping a daily log and sharing it with healthcare providers can guide treatment adjustments.
Medication Adherence
Strict adherence to prescribed medications is essential for managing heart failure. Patients should take their medications as directed, keep a schedule, and discuss any side effects or concerns with their healthcare provider.
Emotional and Mental Health Support
Living with a chronic condition like heart failure can be emotionally challenging. Seeking support from mental health professionals, joining support groups, and staying connected with loved ones can provide emotional relief and improve overall well-being.
Planning for Emergencies
Having a plan in place for emergencies is crucial. This includes knowing when to seek immediate medical attention, having a list of medications and emergency contacts, and understanding the signs of worsening heart failure.
Research And Future Directions
Ongoing research in heart failure aims to develop new treatments and improve outcomes for patients with low EF. Advances in gene therapy, regenerative medicine, and novel drug therapies hold promise for the future. Participation in clinical trials may offer access to cutting-edge treatments and contribute to the advancement of heart failure care.
Conclusion
Living with 20% heart function presents significant challenges, but with appropriate medical management, lifestyle changes, and support, individuals can improve their quality of life and potentially extend their life expectancy. It’s essential for patients to work closely with their healthcare team, stay informed about their condition, and adopt a proactive approach to managing their health. While the prognosis for severe heart failure varies, advancements in treatment and ongoing research continue to offer hope for better outcomes.