Orthostatic hypertension, a condition characterized by a significant increase in blood pressure upon standing, is a lesser-known yet important medical condition that can lead to various health complications. Understanding the underlying causes of orthostatic hypertension is crucial for proper diagnosis and management. In this article, we will delve into the mechanisms behind orthostatic hypertension, explore its symptoms, and discuss its implications. Additionally, we will address a related condition: what causes pulmonary hypertension in infants.
Causes of Orthostatic Hypertension
Several factors can contribute to the development of orthostatic hypertension:
Autonomic Nervous System Dysfunction:
The autonomic nervous system (ANS) regulates involuntary body functions, including heart rate, blood pressure, and digestion.
Dysfunction in the ANS can result in inappropriate blood pressure responses to changes in body position. Disorders such as autonomic neuropathy, often seen in diabetes, can impair the ANS and lead to orthostatic hypertension.
Baroreceptor Sensitivity:
Baroreceptors are specialized cells located in the walls of blood vessels that detect changes in blood pressure and help regulate it. In some individuals, these receptors may become overly sensitive or less effective, causing an exaggerated blood pressure response when standing.
Medications:
Certain medications can influence blood pressure regulation. For instance, medications that increase norepinephrine levels, such as decongestants or certain antidepressants, can exacerbate orthostatic hypertension. Additionally, abrupt discontinuation of antihypertensive drugs can lead to a rebound increase in blood pressure.
Volume Depletion:
Conditions that reduce blood volume, such as dehydration or blood loss, can cause the body to overcompensate when standing, resulting in increased blood pressure. This response is the body’s attempt to ensure adequate blood flow to vital organs despite the reduced blood volume.
Aging:
Aging can affect blood pressure regulation. Older adults may experience changes in vascular stiffness and autonomic function, leading to a higher likelihood of developing orthostatic hypertension.
Underlying Health Conditions:
Conditions such as renal artery stenosis, pheochromocytoma (a rare tumor of the adrenal gland), and primary aldosteronism (a condition causing excess production of aldosterone) can cause or exacerbate orthostatic hypertension.
Implications And Management
Orthostatic hypertension can increase the risk of cardiovascular events, such as stroke and heart attack, due to the persistent elevation in blood pressure. Managing this condition involves addressing the underlying causes and may include lifestyle modifications, medication adjustments, and specific treatments for associated conditions.
Lifestyle Modifications: Maintaining adequate hydration, avoiding rapid changes in position, and wearing compression stockings can help manage symptoms.
Medications: Adjusting or discontinuing medications that exacerbate the condition may be necessary. In some cases, medications to control blood pressure, such as alpha-blockers or beta-blockers, may be prescribed.
Treating Underlying Conditions: Managing conditions like diabetes, renal artery stenosis, or pheochromocytoma can alleviate symptoms of orthostatic hypertension.
What Causes Pulmonary Hypertension in Infants
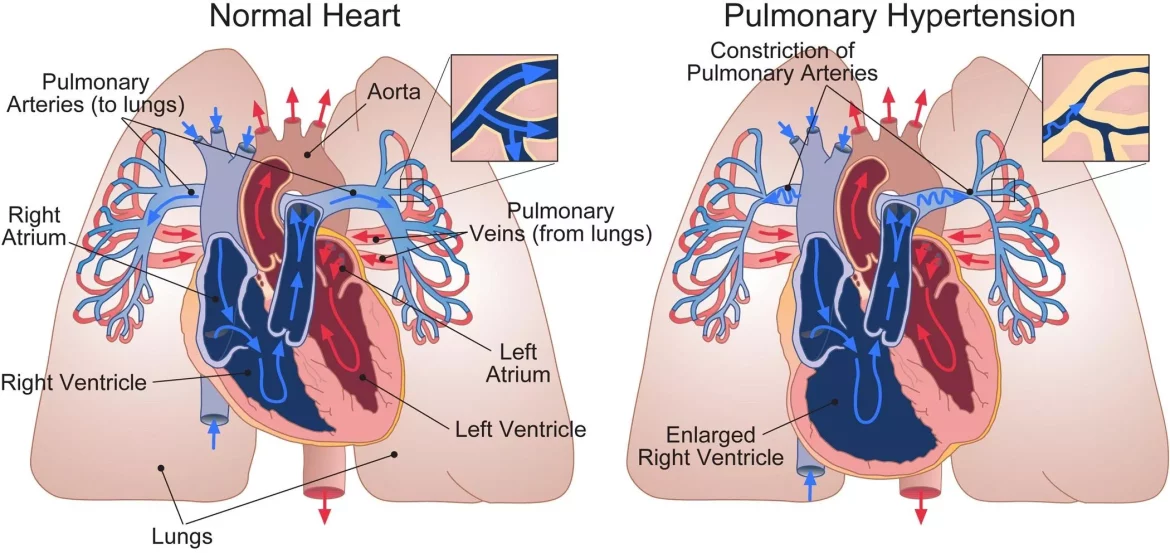
Pulmonary hypertension (PH) in infants is a serious condition characterized by high blood pressure in the arteries of the lungs. This condition can severely impact an infant’s ability to breathe and obtain adequate oxygen. Understanding the causes of pulmonary hypertension in infants is essential for timely diagnosis and treatment.
Common Causes of Pulmonary Hypertension in Infants
Congenital Heart Defects:
Infants with congenital heart defects, such as ventricular septal defects (VSD) or atrial septal defects (ASD), are at higher risk of developing pulmonary hypertension.
These defects can cause abnormal blood flow between the heart chambers, leading to increased pressure in the pulmonary arteries.
Premature Birth:
Premature infants often have underdeveloped lungs, which can result in chronic lung disease and subsequent pulmonary hypertension.
Conditions such as bronchopulmonary dysplasia (BPD) are commonly seen in premature infants and can contribute to the development of PH.
Persistent Pulmonary Hypertension of the Newborn (PPHN):
PPHN is a condition where a newborn’s circulation system does not adapt to breathing outside the womb. This results in persistently high blood pressure in the lungs and inadequate oxygenation. PPHN can be caused by factors such as meconium aspiration, infection, or birth asphyxia.
Genetic and Metabolic Disorders:
Certain genetic conditions, such as Down syndrome, can increase the risk of pulmonary hypertension in infants. Metabolic disorders that affect the lungs or heart can also contribute to the development of PH.
Chronic Lung Diseases:
Conditions like cystic fibrosis or interstitial lung disease can cause chronic inflammation and scarring in the lungs, leading to increased pulmonary artery pressure.
Infections:
Severe respiratory infections, such as respiratory syncytial virus (RSV) or pneumonia, can damage the lung tissue and lead to pulmonary hypertension.
Symptoms And Diagnosis in Infants
The symptoms of pulmonary hypertension in infants can include:
- Rapid breathing or difficulty breathing
- Cyanosis (a bluish tint to the skin, lips, or nail beds)
- Poor feeding or failure to thrive
- Irritability or lethargy
- Swelling in the legs, abdomen, or around the eyes
Diagnosis of pulmonary hypertension in infants typically involves echocardiography to visualize the heart and measure the pressure in the pulmonary arteries. Additional tests may include blood tests, chest X-rays, and cardiac catheterization.
Management And Treatment
The treatment of pulmonary hypertension in infants focuses on addressing the underlying cause and managing the symptoms:
Oxygen Therapy: Providing supplemental oxygen can help improve oxygen levels in the blood and reduce the strain on the heart.
Medications: Vasodilators, such as sildenafil or nitric oxide, can help relax the pulmonary arteries and lower blood pressure. Diuretics may be used to reduce fluid buildup.
Surgery: In cases where a congenital heart defect is the cause, surgical intervention may be necessary to correct the defect.
Supportive Care: Ensuring adequate nutrition and monitoring for complications are essential components of managing PH in infants.
Conclusion
Orthostatic hypertension and pulmonary hypertension in infants are distinct conditions with serious health implications.
Understanding the causes, symptoms, and management strategies for each is crucial for effective treatment. While orthostatic hypertension primarily affects adults and involves an abnormal increase in blood pressure upon standing, pulmonary hypertension in infants results from various congenital, genetic, and environmental factors that lead to high blood pressure in the lungs. Early diagnosis and targeted treatment are essential for improving outcomes and quality of life for those affected by these conditions.