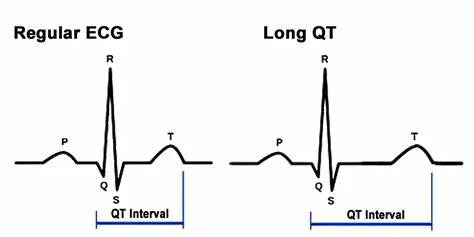
A prolonged QT interval is a significant indicator of potential cardiac issues. The QT interval on an electrocardiogram (ECG) represents the time it takes for the heart’s ventricles to depolarize and then repolarize.
Essentially, it is the duration from the start of the Q wave to the end of the T wave. When this interval is extended beyond the normal range, it is referred to as a prolonged or long QT interval, and it can be a marker for serious and potentially life-threatening heart conditions.
Understanding The QT Interval
To fully grasp why a long QT interval is dangerous, it is essential to understand the basics of cardiac electrophysiology. The heart’s electrical system controls the sequence of events involved in the cardiac cycle, ensuring that the heart beats in a coordinated and efficient manner.
Q Wave: Represents the initial depolarization of the interventricular septum.
R Wave: Corresponds to the depolarization of the main mass of the ventricles.
S Wave: Represents the final depolarization of the ventricles at the base of the heart.
T Wave: Reflects the repolarization of the ventricles.
The QT interval encompasses the entire process of ventricular depolarization and repolarization. A normal QT interval varies depending on age, sex, and heart rate, but it generally ranges from 350 to 450 milliseconds.
See Also: Beta Blockers Cause Palpitations
Why Is A Long QT Interval Dangerous?
Increased Risk of Torsades de Pointes
A long QT interval is primarily dangerous because it can predispose individuals to a specific type of abnormal heart rhythm called Torsades de Pointes (TdP). TdP is a form of polymorphic ventricular tachycardia that can degenerate into ventricular fibrillation, leading to sudden cardiac arrest.
Mechanism: In TdP, the elongated QT interval creates an environment where early afterdepolarizations (EADs) can occur.
EADs are abnormal depolarizations during phase 2 or 3 of the action potential and can trigger a premature heartbeat.
Outcome: When multiple EADs occur, they can lead to a rapid and chaotic heart rhythm characteristic of TdP. If not promptly treated, TdP can progress to ventricular fibrillation, a condition where the heart quivers ineffectively, stopping blood circulation and leading to sudden cardiac death.
Syncope and Sudden Death
Individuals with a prolonged QT interval are at a higher risk of experiencing syncope (fainting) or sudden cardiac death.
These events often occur without warning and can be triggered by physical exertion, stress, or even during sleep.
Syncope: The abnormal heart rhythms associated with a long QT interval can lead to a sudden drop in blood pressure, resulting in fainting.
Sudden Death: In severe cases, the abnormal rhythm does not correct itself, leading to a complete cessation of effective heart function.
Triggers and Exacerbating Factors
Several factors can exacerbate the risks associated with a long QT interval:
Medications: Certain medications, including antiarrhythmics, antidepressants, antipsychotics, and some antibiotics, can prolong the QT interval.
Electrolyte Imbalances: Low levels of potassium, magnesium, or calcium can increase the risk of a prolonged QT interval.
Genetics: Congenital long QT syndrome (LQTS) is a genetic disorder that affects the ion channels in the heart, leading to prolonged repolarization.
Congenital Long QT Syndrome (LQTS)
Congenital LQTS is a genetic condition that affects the heart’s ion channels. There are several types of LQTS, each associated with mutations in different genes responsible for the proper functioning of ion channels.
LQT1: Most commonly caused by mutations in the KCNQ1 gene, affecting potassium channels.
LQT2: Linked to mutations in the KCNH2 gene, also affecting potassium channels.
LQT3: Caused by mutations in the SCN5A gene, which affects sodium channels.
see also: why is afib with rvr dangerous
Acquired Long QT Syndrome
Acquired long QT syndrome can result from various external factors:
Medications: As mentioned, many drugs can prolong the QT interval.
Electrolyte Imbalances: Conditions that cause imbalances in blood electrolytes, such as severe diarrhea or vomiting, can prolong the QT interval.
Other Medical Conditions: Certain diseases, such as heart failure, can also lead to a prolonged QT interval.
Diagnosis And Monitoring
Diagnosing a long QT interval typically involves an electrocardiogram (ECG), where the QT interval is measured and corrected for heart rate (QTc). A QTc greater than 450 milliseconds in men and 460 milliseconds in women is generally considered prolonged.
Holter Monitoring: Continuous ECG monitoring over 24 to 48 hours can help identify intermittent prolongation of the QT interval and associated arrhythmias.
Genetic Testing: For individuals with suspected congenital LQTS, genetic testing can identify specific mutations associated with the condition.
Management And Treatment
Managing a long QT interval focuses on reducing the risk of TdP and other serious arrhythmias:
Avoiding Triggers: Patients are advised to avoid medications and conditions that can prolong the QT interval.
Medications: Beta-blockers are commonly prescribed to reduce the risk of arrhythmias in patients with LQTS.
Lifestyle Changes: Patients are encouraged to avoid strenuous activities and stress, which can trigger arrhythmias.
Implantable Cardioverter-Defibrillator (ICD): In high-risk patients, an ICD may be implanted to detect and correct life-threatening arrhythmias.
Prognosis
With proper management, many individuals with a prolonged QT interval can lead normal lives. However, the prognosis varies depending on the underlying cause and the presence of other risk factors. Early detection and intervention are crucial in reducing the risk of sudden cardiac death.
Conclusion
Understanding why a long QT interval is dangerous is crucial for both patients and healthcare providers. The prolonged QT interval signifies a predisposition to potentially fatal arrhythmias like Torsades de Pointes and sudden cardiac death.
Awareness of the condition, appropriate diagnosis, and management strategies are essential in mitigating the associated risks and improving patient outcomes. With advancements in genetic testing and personalized medicine, the ability to identify and treat individuals with prolonged QT intervals continues to improve, offering hope for those affected by this serious condition.