Heart failure is a complex clinical syndrome resulting from any structural or functional impairment of ventricular filling or ejection of blood. It is a leading cause of morbidity and mortality worldwide, and understanding its different types is crucial for effective diagnosis and treatment. This article explores the six most common types of heart failure, delving into their causes, symptoms, diagnostic criteria, and treatment options.
1. Heart Failure with Reduced Ejection Fraction (HFrEF)
Understanding HFrEF
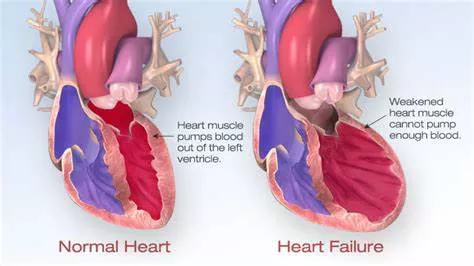
Heart Failure with Reduced Ejection Fraction (HFrEF), also known as systolic heart failure, occurs when the heart muscle is unable to contract effectively, resulting in a reduced ejection fraction (EF) of less than 40%. This condition impairs the heart’s ability to pump blood efficiently, leading to inadequate perfusion of the body’s tissues.
Causes
The primary causes of HFrEF include:
Coronary Artery Disease (CAD): Blocked or narrowed arteries reduce blood flow to the heart muscle.
Myocardial Infarction (Heart Attack): Damage to the heart muscle from a heart attack weakens its pumping ability.
Hypertension: Chronic high blood pressure forces the heart to work harder, leading to muscle weakness.
Cardiomyopathy: Diseases affecting the heart muscle, such as dilated cardiomyopathy, reduce its contractility.
see also: What Does A Cardiac Cough Feel Like
Symptoms
Common symptoms of HFrEF include:
- Shortness of breath, especially during exertion or when lying flat
- Fatigue and weakness
- Swelling in the legs, ankles, and feet
- Rapid or irregular heartbeat
- Persistent cough or wheezing due to fluid buildup in the lungs
Diagnosis and Treatment
Diagnosis typically involves an echocardiogram to measure the ejection fraction, along with other tests like ECG, chest X ray, and blood tests. Treatment options include:
Medications: ACE inhibitors, beta-blockers, diuretics, and aldosterone antagonists.
Lifestyle Changes: Diet modification, exercise, smoking cessation, and weight management.
Devices and Surgery: Implantable cardioverter-defibrillators (ICDs), cardiac resynchronization therapy (CRT), and, in severe cases, heart transplants.
2. Heart Failure with Preserved Ejection Fraction (HFpEF)
Understanding HFpEF
Heart Failure with Preserved Ejection Fraction (HFpEF), or diastolic heart failure, occurs when the heart muscle contracts normally but is stiff or thickened, impairing its ability to relax and fill with blood. The ejection fraction remains normal (50% or higher), but the heart cannot fill adequately, leading to symptoms of heart failure.
Causes
Common causes of HFpEF include:
Hypertension: Long-term high blood pressure can cause the heart muscle to thicken and stiffen.
Aging: The heart becomes less compliant with age.
Diabetes: Can lead to changes in the heart muscle.
Obesity: Increases the risk of developing HFpEF.
see also: Signs of Right Sided Heart Failure Include
Symptoms
Symptoms of HFpEF are similar to those of HFrEF:
- Shortness of breath
- Fatigue
- Swelling in the lower extremities
- Difficulty exercising
- Diagnosis and Treatment
Diagnosis involves echocardiography and tests to assess heart stiffness. Treatment focuses on managing underlying conditions and symptoms:
Medications: Diuretics to manage fluid retention, antihypertensives, and medications to control heart rate.
Lifestyle Changes: Weight management, exercise, and dietary modifications.
Management of Comorbidities: Addressing conditions like hypertension and diabetes is crucial.
3. Left-Sided Heart Failure
Understanding Left-Sided Heart Failure
Left-sided heart failure is the most common form and occurs when the left ventricle cannot pump blood effectively to the body. It can lead to fluid buildup in the lungs (pulmonary congestion).
Causes
Causes of left-sided heart failure include:
Coronary Artery Disease: Reduces blood flow to the left ventricle.
Hypertension: Increases the workload on the left ventricle.
Valvular Heart Disease: Affects the function of the mitral or aortic valves.
Symptoms
Symptoms include:
- Shortness of breath and difficulty breathing
- Fatigue
- Fluid retention and swelling
- Rapid weight gain from fluid buildup
Diagnosis and Treatment
Diagnosis involves echocardiography, ECG, chest X-rays, and blood tests. Treatment includes:
Medications: ACE inhibitors, beta-blockers, diuretics, and digitalis.
Lifestyle Changes: Diet, exercise, and fluid management.
Surgical Options: Valve repair or replacement, coronary bypass surgery.
4. Right-Sided Heart Failure
Understanding Right-Sided Heart Failure
Right-sided heart failure occurs when the right ventricle cannot pump blood to the lungs efficiently, leading to a backup of blood in the veins and causing swelling and congestion in the lower extremities and abdomen.
Causes
Common causes include:
Left-Sided Heart Failure: Increased pressure in the lungs from left-sided heart failure can strain the right side.
Chronic Lung Diseases: Such as chronic obstructive pulmonary disease (COPD) or pulmonary hypertension.
Pulmonary Embolism: A blood clot in the lungs increases the workload on the right ventricle.
Symptoms
Symptoms include:
- Swelling in the legs, ankles, and feet
- Abdominal swelling and pain
- Frequent urination, especially at night
- Shortness of breath
- Fatigue and weakness
Diagnosis and Treatment
Diagnosis involves echocardiography, ECG, chest X-rays, and blood tests. Treatment focuses on managing symptoms and underlying causes:
Medications: Diuretics, ACE inhibitors, beta-blockers, and medications to manage pulmonary hypertension.
Lifestyle Changes: Diet, exercise, and weight management.
Oxygen Therapy: For patients with chronic lung disease.
5. Congestive Heart Failure (CHF)
Understanding CHF
Congestive Heart Failure (CHF) is a term often used interchangeably with heart failure, but it specifically refers to the stage when fluid builds up around the heart and affects its ability to pump efficiently. CHF can involve either side of the heart or both.
Causes
Causes include:
Coronary Artery Disease: The leading cause of CHF.
Hypertension: Long-term high blood pressure can lead to CHF.
Cardiomyopathy: Diseases affecting the heart muscle.
Valvular Heart Disease: Valve problems can lead to CHF.
Symptoms
Symptoms of CHF include:
- Shortness of breath, particularly when lying down
- Fatigue and weakness
- Swelling in the legs, ankles, and feet
- Rapid or irregular heartbeat
- Persistent cough or wheezing with white or pink-tinged phlegm
Diagnosis and Treatment
Diagnosis involves a thorough physical examination, echocardiography, ECG, chest X-rays, and blood tests. Treatment includes:
Medications: Diuretics, ACE inhibitors, beta-blockers, aldosterone antagonists, and digitalis.
Lifestyle Changes: Diet, exercise, smoking cessation, and fluid management.
Surgical and Device-Based Treatments: ICDs, CRT, valve surgery, and in severe cases, LVAD or heart transplantation.
6. High-Output Heart Failure
Understanding High-Output Heart Failure
High-output heart failure is a less common type where the heart pumps normally or more than normal, but the body’s demand for blood and oxygen exceeds what the heart can supply. It can occur even with a normal or high cardiac output.
Causes
High-output heart failure can be caused by:
Chronic Anemia: Reduces oxygen-carrying capacity, increasing cardiac output.
Hyperthyroidism: Increases metabolic rate and cardiac demand.
Paget’s Disease: Affects bone metabolism and increases blood flow demand.
Arteriovenous Fistula: An abnormal connection between an artery and a vein increases blood flow demand.
Symptoms
Symptoms of high-output heart failure include:
- Shortness of breath
- Fatigue and weakness
- Swelling in the legs, ankles, and feet
- Rapid or irregular heartbeat
- Palpitations
Diagnosis and Treatment
Diagnosis involves blood tests, echocardiography, ECG, and tests for underlying conditions like thyroid function tests and anemia assessment. Treatment focuses on addressing the underlying cause:
Medications: Diuretics, beta-blockers, and treatment for underlying conditions (e.g., thyroid medication).
Lifestyle Changes: Diet, exercise, and managing fluid intake.
Surgical Options: Treating underlying conditions such as arteriovenous fistulas or severe anemia.
Conclusion
Understanding the various types of heart failure is crucial for effective diagnosis and treatment. The six most common types—HFrEF, HFpEF, left-sided heart failure, right-sided heart failure, congestive heart failure, and high-output heart failure—each have distinct causes, symptoms, and treatment approaches. Comprehensive management, including lifestyle modifications, medications, and sometimes surgical interventions, is essential to improve patient outcomes and quality of life. With ongoing research and advancements in medical care, the prognosis for individuals with heart failure continues to improve.