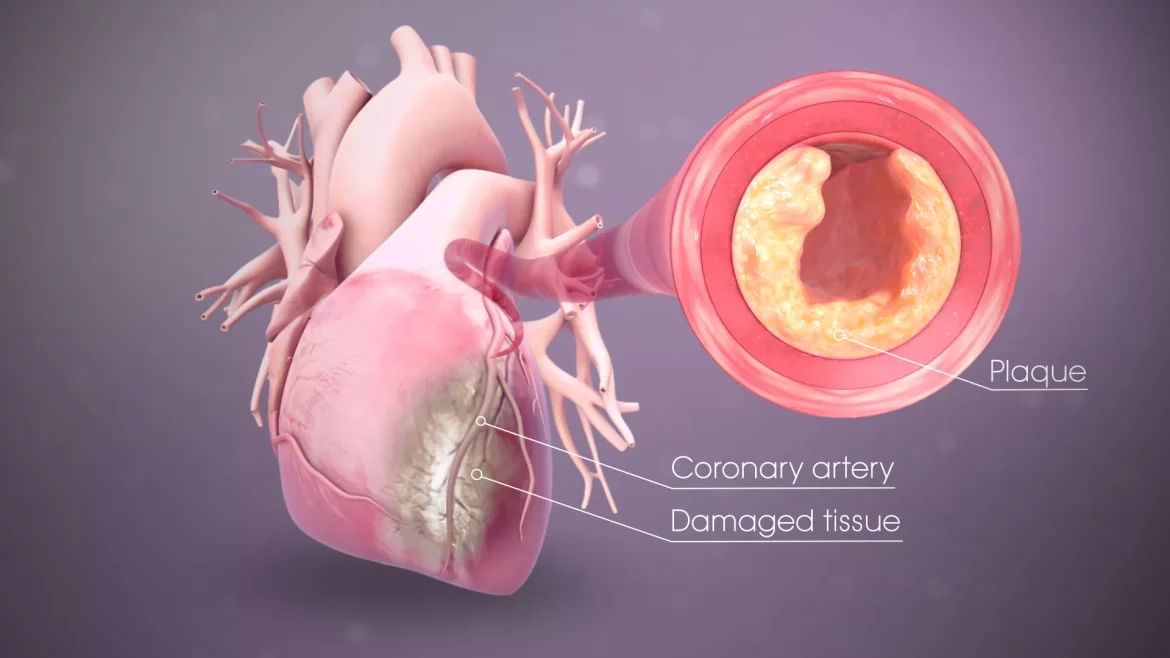
Plaque formation in the heart, a condition known as atherosclerosis, is a critical health issue that can lead to serious cardiovascular diseases, including heart attacks and strokes. This article delves into the intricate process of how plaque forms in the arteries, explores the underlying mechanisms, and discusses the factors that contribute to this potentially life-threatening condition.
The Anatomy of Arteries
To comprehend how plaque forms, it’s essential to understand the basic structure of arteries. Arteries are blood vessels that carry oxygen-rich blood away from the heart to the rest of the body. They have three main layers:
Intima: The innermost layer, which is in direct contact with the blood flow.
Media: The middle layer, composed of smooth muscle cells that provide structural support and elasticity.
Adventitia: The outer layer, consisting of connective tissue that protects and anchors the artery.
Initiation of Plaque Formation
Plaque formation begins with damage to the endothelium, the thin layer of cells lining the inner surface of the arteries. This damage can be caused by several factors:
High Blood Pressure: Increased pressure can harm the endothelial cells.
High Cholesterol: Elevated levels of LDL (low-density lipoprotein) cholesterol can penetrate the endothelium.
Smoking: Chemicals in tobacco smoke can directly damage the endothelial cells.
Diabetes: High blood sugar levels can lead to endothelial dysfunction.
see also: What Are The Symptoms of Blocked Heart Arteries
The Role of LDL Cholesterol
Once the endothelium is damaged, LDL cholesterol particles can enter the artery wall. These LDL particles are then oxidized, which triggers an inflammatory response. The immune system perceives the oxidized LDL as a threat and sends white blood cells called macrophages to engulf and digest the LDL.
Formation of Fatty Streaks
As macrophages consume the oxidized LDL, they transform into foam cells. These foam cells accumulate in the intima, forming fatty streaks, which are the earliest visible signs of atherosclerosis. Fatty streaks are common in young individuals and may not cause any immediate symptoms.
Plaque Progression
Over time, the accumulation of foam cells and other inflammatory cells leads to the formation of a fibrous cap. This cap is composed of smooth muscle cells and collagen, which attempts to stabilize the plaque. However, the continued deposition of lipids, calcium, and cellular debris within the plaque can cause it to grow and thicken the arterial wall.
Complicated Plaque
As the plaque progresses, it can become unstable. Factors contributing to plaque instability include:
Inflammation: Chronic inflammation can weaken the fibrous cap.
Calcification: The deposition of calcium can make the plaque brittle.
Thinning of the Fibrous Cap: A thin cap is more likely to rupture.
Rupture And Thrombosis
The most dangerous phase of plaque formation occurs when the fibrous cap ruptures. This exposes the inner contents of the plaque to the bloodstream, triggering the formation of a blood clot (thrombus). A thrombus can partially or completely block blood flow in the affected artery, leading to conditions such as:
Myocardial Infarction (Heart Attack): If a coronary artery is blocked, the heart muscle can be deprived of oxygen, causing a heart attack.
Ischemic Stroke: If a carotid artery is blocked, it can lead to a stroke due to reduced blood flow to the brain.
Risk Factors for Plaque Formation
Several risk factors increase the likelihood of plaque formation in the heart:
Genetics: Family history of heart disease can predispose individuals to atherosclerosis.
Age: The risk increases with age as arterial walls naturally thicken and lose elasticity.
Gender: Men are at higher risk at a younger age, although the risk for women increases post-menopause.
Lifestyle Factors: Poor diet, lack of physical activity, obesity, and excessive alcohol consumption can all contribute to plaque formation.
Preventive Measures
Preventing plaque formation involves addressing modifiable risk factors:
Healthy Diet: Consuming a diet low in saturated fats, trans fats, and cholesterol can help reduce LDL levels.
Regular Exercise: Physical activity helps improve overall cardiovascular health and lowers blood pressure.
Smoking Cessation: Quitting smoking significantly reduces the risk of atherosclerosis.
Managing Diabetes: Controlling blood sugar levels can prevent endothelial damage.
Medical Interventions
For those at high risk or already experiencing symptoms, medical interventions may be necessary:
Medications: Statins, aspirin, and blood pressure medications can help manage cholesterol levels and reduce inflammation.
Surgical Procedures: In severe cases, procedures such as angioplasty or coronary artery bypass grafting (CABG) may be required to restore blood flow.
Conclusion
Plaque formation in the heart is a complex process that begins with endothelial damage and progresses through various stages, ultimately leading to potential life-threatening conditions if left unchecked. Understanding the mechanisms and risk factors involved is crucial for prevention and management. By adopting a healthy lifestyle and, when necessary, seeking medical intervention, individuals can significantly reduce their risk of developing atherosclerosis and its associated complications.
In summary, the formation of plaque in the heart is a dynamic and multifaceted process influenced by a combination of genetic, environmental, and lifestyle factors. Effective prevention and treatment strategies are essential to combat the prevalence of cardiovascular diseases and improve overall heart health.