In recent years, the medical community has witnessed significant shifts in the approach to managing blood pressure, crucial for reducing the risk of heart disease, stroke, and other health complications. The latest updates to blood pressure (BP) guidelines mark a significant change in how hypertension is diagnosed and managed. This article explores the nuances of the new BP guidelines, the rationale behind these changes, and their implications for both healthcare providers and patients.
Background And Rationale for Change
High blood pressure, or hypertension, is a major risk factor for cardiovascular diseases and a significant public health concern globally. Traditionally, hypertension has been defined as a blood pressure reading of 140/90 mmHg or higher.
However, recent research has shown that damage to blood vessels and the heart can occur at lower levels than previously understood. This evidence prompted a reevaluation of the threshold for what constitutes high blood pressure.
In 2017, the American College of Cardiology (ACC) and the American Heart Association (AHA) updated their guidelines, lowering the threshold for hypertension to 130/80 mmHg. This change means more individuals are classified as having high blood pressure, with the goal of initiating earlier intervention to prevent cardiovascular events.
see also: 8 Herbal Teas That Can Reduce High Blood Pressure You May Not Know
Detailed Breakdown of The New Guidelines
The 2017 ACC/AHA guidelines for the management of hypertension include several key updates:
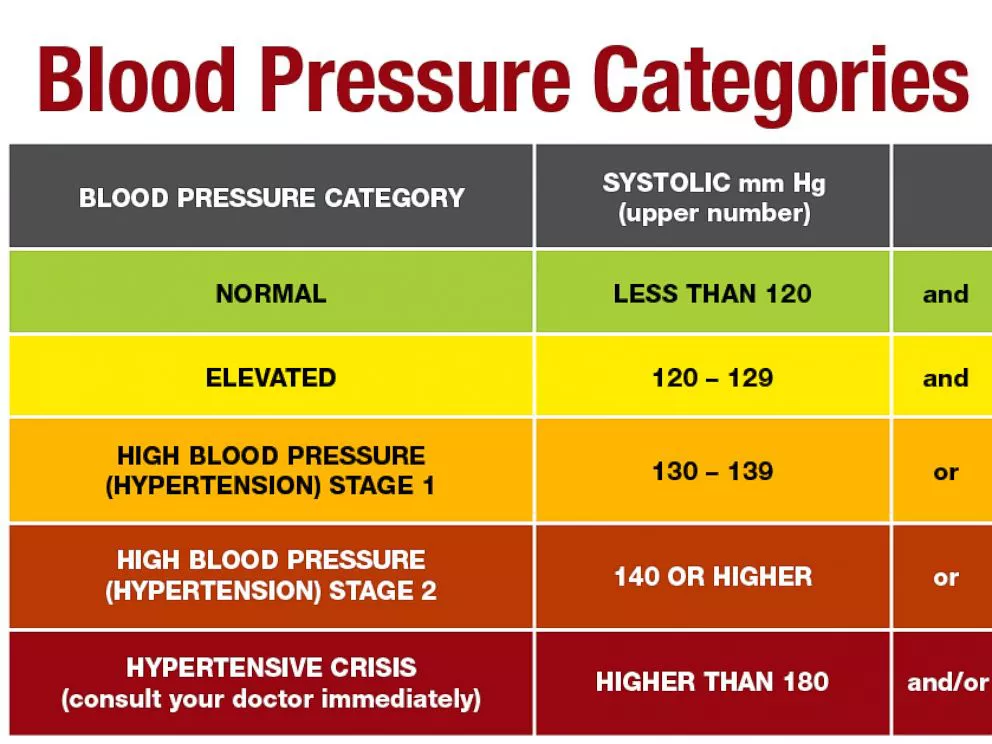
Definition of Hypertension: The threshold for stage 1 hypertension is now set at 130-139/80-89 mmHg, and stage 2 hypertension is defined as 140/90 mmHg or higher.
Risk Assessment: The new guidelines emphasize the importance of assessing cardiovascular risk factors when diagnosing and treating hypertension. A comprehensive risk assessment includes looking at family history, lifestyle factors, and the presence of other conditions such as diabetes or kidney disease.
Lifestyle Changes: There is a stronger emphasis on lifestyle modifications as a first line of treatment. Recommended changes include adopting a heart-healthy diet (rich in fruits, vegetables, whole grains, and low in saturated fats and cholesterol), increasing physical activity, reducing sodium intake, limiting alcohol consumption, and maintaining a healthy weight.
Medication Management: For those with stage 1 hypertension who have already experienced a cardiovascular event or are at high risk of heart disease, medication is generally recommended in addition to lifestyle changes. The choice of medication and treatment targets can vary based on individual patient factors.
Monitoring and Follow-up: The guidelines recommend more frequent follow-ups for individuals with elevated blood pressure readings. This approach helps ensure that treatment adjustments can be made timely to achieve optimal blood pressure control.
Implications for Healthcare Providers
The updated guidelines necessitate a shift in practice for many healthcare providers. With the lower threshold for hypertension diagnosis, more patients will require monitoring and potentially medication management. Healthcare providers need to be well-versed in the new guidelines and capable of implementing them effectively.
1. Education and Training: Medical professionals may need additional training to understand and apply the new guidelines correctly. This training should cover how to measure blood pressure accurately, interpret the results within the new framework, and implement risk assessment strategies.
2. Patient Communication: Providers must also excel in patient communication to explain the changes in the guidelines and what they mean for individual treatment plans. Patients may be concerned about being diagnosed with hypertension earlier than they might have been under the old guidelines. Clear communication can help alleviate these concerns and emphasize the benefits of early intervention.
3. Technology and Tools: Utilizing technology, such as electronic health records (EHRs) and patient management systems, can help track and manage patient data more efficiently. Tools that support decision-making in hypertension management can also aid providers in following the new guidelines.
See Also: 5 Types of Juices Good for High Blood Pressure You May Not Know
Implications for Patients
For patients, the new guidelines mean that earlier intervention may be necessary. This early approach aims to prevent the progression of hypertension and associated complications.
1. Awareness and Education: Patients need to understand what the new blood pressure numbers mean and the importance of maintaining blood pressure within the recommended range. Education about the role of lifestyle factors in controlling blood pressure is also crucial.
2. Active Participation: With the emphasis on lifestyle changes, patients have a more active role in managing their health.
This involvement includes adhering to dietary recommendations, participating in regular physical activity, and monitoring blood pressure at home.
3. Healthcare Engagement: Regular check-ups and more frequent monitoring are recommended under the new guidelines. Patients should be prepared to engage more regularly with their healthcare providers, which can help in adjusting treatment plans promptly based on blood pressure readings.
Conclusion
The new blood pressure guidelines represent a significant shift towards earlier intervention and more stringent management of blood pressure. By lowering the threshold for hypertension, these guidelines aim to reduce the incidence of cardiovascular disease and improve overall public health outcomes. Both healthcare providers and patients must adapt to these changes, emphasizing education, effective communication, and the use of technological tools to manage hypertension more effectively. As research continues to evolve, these guidelines may be subject to further adjustments, highlighting the dynamic nature of medical science and the continuous effort to enhance patient care in the face of changing health landscapes.
FAQs
Is 140/90 the new normal?
No, 140/90 mmHg is no longer considered the “new normal” for blood pressure. As per the 2017 guidelines from the American College of Cardiology (ACC) and the American Heart Association (AHA), the threshold for hypertension has been lowered to 130/80 mmHg. Blood pressure readings of 140/90 mmHg or higher are now classified as stage 2 hypertension.
This update was made to encourage earlier intervention and management to prevent cardiovascular disease and other complications associated with higher blood pressure levels.
What are the new guidelines for measuring blood pressure?
The new guidelines emphasize the importance of accurate blood pressure measurement to ensure reliable readings and appropriate management. Key points include:
Preparation: Patients should avoid caffeine, exercise, and smoking at least 30 minutes before measurement. They should also have at least 5 minutes of rest in a quiet environment before taking a reading.
Positioning: During the measurement, the patient should be seated with their back supported, feet flat on the floor, and arms supported at heart level. The blood pressure cuff should be placed on a bare arm.
Equipment: It is recommended to use a validated, calibrated device for blood pressure measurement. The cuff size should be appropriate for the patient’s arm circumference to ensure accuracy.
Technique: Two readings should be taken, at least 1 to 2 minutes apart, and additional readings if the first two differ significantly. The average of these readings should be used to determine the patient’s blood pressure status.
Frequency: Regular monitoring, as recommended by a healthcare provider, is crucial, especially for individuals with high blood pressure or those at risk.
What is the new normal blood pressure for seniors?
The new guidelines do not specify a different “normal” blood pressure for seniors but do acknowledge that a slightly higher systolic blood pressure may be acceptable depending on individual health conditions and overall risk factors. For most older adults, the target blood pressure remains below 130/80 mmHg. However, treatment goals can be adjusted based on a comprehensive health assessment and the presence of conditions like frailty or multiple chronic conditions.
For seniors, the emphasis is also placed on the careful management of blood pressure medications to avoid side effects, such as dizziness and falls, which are more prevalent in older populations. The decision to initiate or adjust medication should always be tailored to the individual, considering both the potential benefits and risks of treatment. Healthcare providers often take a more conservative approach to blood pressure targets and treatment in very elderly patients or those with significant comorbidities.