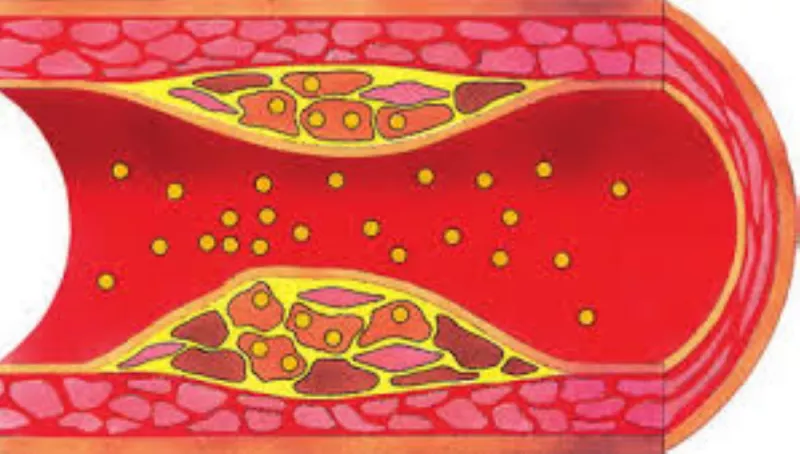
Hyperlipidemia, a medical condition characterized by elevated levels of lipids (fats) in the blood, is a major risk factor for cardiovascular diseases. These lipids include cholesterol and triglycerides, which are crucial for various bodily functions but can become detrimental when present in excess. Diagnosing hyperlipidemia early is essential for preventing complications such as heart attacks, strokes, and atherosclerosis. This article delves into the process of diagnosing hyperlipidemia, including the necessary tests, interpretation of results, and the importance of regular monitoring.
Clinical Symptoms And Risk Factors
Hyperlipidemia often presents no obvious symptoms, making routine screening and diagnosis essential. However, certain risk factors can increase the likelihood of developing hyperlipidemia:
Genetic Predisposition: Family history of hyperlipidemia or cardiovascular diseases.
Lifestyle Factors: Poor diet, lack of physical activity, smoking, and excessive alcohol consumption.
Medical Conditions: Obesity, diabetes, hypothyroidism, and chronic kidney disease.
Age and Gender: Risk increases with age, and men are generally at higher risk until women reach menopause.
Given the asymptomatic nature of hyperlipidemia, these risk factors should prompt individuals and healthcare providers to prioritize lipid level screening.
Diagnostic Procedures for Hyperlipidemia
1. Initial Clinical Assessment:
The first step in diagnosing hyperlipidemia involves a thorough clinical assessment. This includes:
Medical History: Assessing the patient’s medical history, including any family history of hyperlipidemia or cardiovascular diseases.
Physical Examination: Checking for physical signs that might indicate lipid abnormalities, such as xanthomas (fat deposits under the skin) or corneal arcus (a white or gray ring around the cornea).
see also: What Symptoms Are Associated with Hyperlipidemia
2. Lipid Profile Testing:
The definitive diagnosis of hyperlipidemia is made through blood tests known as lipid profiles or lipid panels. These tests measure the levels of various lipids in the blood, providing a comprehensive overview of a patient’s lipid status. A typical lipid profile includes:
Total Cholesterol: The overall level of cholesterol in the blood.
LDL Cholesterol: The amount of low-density lipoprotein cholesterol.
HDL Cholesterol: The level of high-density lipoprotein cholesterol.
Triglycerides: The total amount of triglycerides.
3. Fasting vs. Non-Fasting Lipid Profiles:
Traditionally, lipid profile tests require fasting for 9-12 hours to avoid the impact of recent food intake on triglyceride levels.
However, recent guidelines suggest that non-fasting lipid profiles can also provide accurate and valuable information, particularly for initial screenings.
4. Interpreting Lipid Profile Results:
The interpretation of lipid profile results involves comparing the measured levels with established reference ranges.
The American Heart Association (AHA) provides the following general guidelines for lipid levels:
Total Cholesterol:
- Desirable: Less than 200 mg/dL
- Borderline High: 200-239 mg/dL
- High: 240 mg/dL and above
LDL Cholesterol:
Optimal: Less than 100 mg/dL
Near Optimal/Above Optimal: 100-129 mg/dL
Borderline High: 130-159 mg/dL
High: 160-189 mg/dL
Very High: 190 mg/dL and above
HDL Cholesterol:
- Low (Poor): Less than 40 mg/dL (for men) or less than 50 mg/dL (for women)
- High (Good): 60 mg/dL and above
Triglycerides:
- Normal: Less than 150 mg/dL
- Borderline High: 150-199 mg/dL
- High: 200-499 mg/dL
- Very High: 500 mg/dL and above
5. Advanced Lipoprotein Testing:
In some cases, basic lipid profiles might not provide sufficient information, especially for individuals with borderline or conflicting results. Advanced lipoprotein testing can offer more detailed insights into lipid particles and their behavior.
These tests include:
Apolipoprotein B (ApoB): Measures the number of LDL particles, providing a more accurate assessment of cardiovascular risk than LDL-C alone.
Lipoprotein(a) [Lp(a)]: A genetic variant of LDL associated with increased cardiovascular risk.
Nuclear Magnetic Resonance (NMR) Spectroscopy: Provides detailed information about lipoprotein particle size and concentration.
6. Genetic Testing:
For individuals with a strong family history of hyperlipidemia or those diagnosed at a young age, genetic testing can identify specific mutations responsible for inherited forms of the condition, such as familial hypercholesterolemia. Identifying these mutations can help tailor treatment and management strategies.
7. Additional Diagnostic Considerations:
While lipid profiles are the cornerstone of hyperlipidemia diagnosis, other tests and factors can play a role in comprehensive cardiovascular risk assessment. These include:
Blood Glucose Levels: To assess for diabetes or prediabetes, which often coexists with hyperlipidemia.
Liver Function Tests: Since some lipid-lowering medications can affect liver function.
Thyroid Function Tests: Hypothyroidism can contribute to elevated cholesterol levels.
8. Lifestyle and Dietary Assessment:
Assessing a patient’s lifestyle and dietary habits is also crucial in diagnosing and managing hyperlipidemia. Healthcare providers should discuss:
Diet: The intake of saturated fats, trans fats, cholesterol, and refined sugars.
Physical Activity: Frequency, intensity, and type of exercise.
Smoking and Alcohol Use: Both can negatively impact lipid levels and overall cardiovascular health.
9. Ongoing Monitoring and Follow-Up:
Diagnosing hyperlipidemia is not a one-time event. Regular monitoring and follow-up are essential to track the effectiveness of treatment and make necessary adjustments. This typically involves:
Periodic Lipid Profile Testing: To monitor changes in lipid levels and assess the response to lifestyle modifications or medications.
Continuous Risk Assessment: Evaluating changes in cardiovascular risk factors and overall health status.
Treatment And Management Strategies
Once hyperlipidemia is diagnosed, the primary goal is to reduce cardiovascular risk through lifestyle modifications and, if necessary, medications. Treatment strategies include:
Dietary Changes: Emphasizing a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats while reducing the intake of saturated fats, trans fats, and cholesterol.
Physical Activity: Engaging in regular aerobic exercise, such as walking, running, or cycling, for at least 150 minutes per week.
Weight Management: Achieving and maintaining a healthy weight through diet and exercise.
Smoking Cessation: Eliminating tobacco use to improve lipid levels and overall cardiovascular health.
Medications: Statins, fibrates, niacin, and other lipid-lowering drugs may be prescribed to achieve target lipid levels.
Conclusion
Diagnosing hyperlipidemia involves a multifaceted approach, including clinical assessment, lipid profile testing, advanced lipoprotein analysis, and lifestyle evaluation. Early detection and regular monitoring are crucial for effective management and prevention of cardiovascular diseases. By understanding the diagnostic process and taking proactive steps to maintain healthy lipid levels, individuals can significantly reduce their risk of heart disease and improve their overall health and well-being.