To fully grasp what postural drop involves, it’s important to understand some basic human physiology. Blood pressure is the force exerted by circulating blood on the walls of blood vessels. It is one of the critical parameters that is regulated by the autonomic nervous system, which controls involuntary actions of the body such as heartbeat and dilation or constriction of blood vessels.
When a person changes position from lying down to standing, gravity causes blood to pool in the veins of the legs and lower body. In a healthy individual, the body compensates for this by increasing the heart rate, constricting blood vessels, and activating volume receptors to maintain blood flow to the brain and vital organs. However, in individuals with postural drop, these mechanisms are delayed, insufficient, or fail entirely, leading to a significant decrease in blood pressure and subsequent symptoms.
What Is Postural Drop?
Postural drop, also known as orthostatic hypotension or postural hypotension, is a form of low blood pressure that happens when a person stands up from sitting or lying down. This condition can cause dizziness, lightheadedness, fainting, and even falls, presenting significant risks especially in older adults. Understanding postural drop is crucial not only for those directly affected but also for caregivers, healthcare providers, and anyone involved in the care of vulnerable populations.
See Also: How to Prevention The Hypertension
Causes of Postural Drop
The causes of postural drop are diverse and can include factors such as:
Aging: Natural changes in blood pressure regulation as people age can make postural drop more common in elderly populations.
Medications: Many medications, especially those used to treat high blood pressure, heart conditions, and Parkinson’s disease, can exacerbate or cause symptoms of postural drop.
Dehydration: Inadequate fluid intake leads to lower blood volume, which can precipitate a drop in blood pressure upon standing.
Neurological conditions: Diseases such as Parkinson’s disease, multiple system atrophy, and diabetic neuropathy can impair the autonomic nervous system’s ability to regulate blood pressure.
Heart problems: Conditions like heart valve problems, heart failure, or very low heart rate can prevent the body from adequately adjusting blood pressure.
Endocrine disorders: Issues such as adrenal insufficiency and diabetes can affect blood pressure control.
Prolonged bed rest: Extended periods of immobility can reduce the body’s ability to regulate blood pressure effectively.
Symptoms And Diagnosis
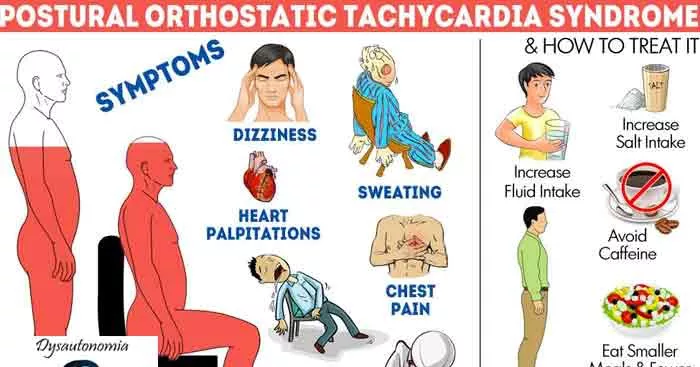
The primary symptom of postural drop is a sudden feeling of dizziness or lightheadedness upon standing, which may resolve after a few seconds or minutes as the body adapts. In severe cases, it can lead to fainting, confusion, blurred vision, or falls. These symptoms can cause significant distress and impact the quality of life, making diagnosis and management crucial.
Diagnosing postural drop involves measuring blood pressure while the patient is lying down and then again several times after standing. A typical diagnostic criterion is a drop of at least 20 mm Hg in systolic blood pressure or at least 10 mm Hg in diastolic blood pressure within three minutes of standing. Healthcare providers may also perform tests to rule out other causes of fainting or dizziness, and review medications that could contribute to the symptoms.
Management And Treatment
Managing postural drop focuses on reducing symptoms and preventing injuries from falls. Treatment strategies include:
Lifestyle modifications: Simple changes such as rising slowly from a seated or lying position, avoiding large meals that can divert blood flow to the intestines, and increasing water and salt intake (if not contraindicated by other conditions) can help.
Physical countermeasures: Compression stockings and abdominal binders can help prevent blood from pooling in the legs. Physical exercises that strengthen the leg muscles and improve venous return are also beneficial.
Medication adjustments: Reviewing and adjusting medications that may exacerbate postural drop is a critical step. In some cases, medications might be added to increase blood volume or constrict blood vessels.
Education and support: Educating patients and caregivers about the signs, symptoms, and management of postural drop is essential for preventing falls and injuries.
Prevention And Long-term Care
Preventive measures for postural drop are particularly important for those at higher risk, such as the elderly or those with significant medical comorbidities. Regular physical activity, adequate hydration, and regular medical check-ups can play a key role in preventing episodes. For those who experience frequent and severe symptoms, ongoing medical care may be required, and in some cases, referral to a specialist in cardiovascular or neurological disorders might be necessary.
Conclusion
Postural drop is a complex condition with potentially serious consequences but can often be managed effectively with a combination of lifestyle adjustments, medical treatment, and patient education. Understanding this condition helps in early recognition and prevention of complications, thereby improving the quality of life for those affected. As research continues to evolve, further insights will likely aid in the development of more effective management strategies for postural drop.
In-depth understanding and management of postural drop are crucial, not just for those directly affected, but for healthcare providers and caregivers involved in the care of at-risk populations, ensuring improved outcomes and better overall health management.