Atrial fibrillation (AFib) is the most common type of irregular heartbeat (arrhythmia), characterized by rapid and erratic electrical signals in the atria, the heart’s upper chambers. Effective management of AFib is crucial to prevent complications such as stroke, heart failure, and other cardiovascular issues. This article explores the comprehensive treatment approach for atrial fibrillation, focusing on what to give for AFib to ensure optimal patient outcomes.
Understanding Atrial Fibrillation
Atrial fibrillation occurs when the heart’s normal rhythm is disrupted, causing the atria to quiver instead of contracting efficiently. This leads to an irregular and often rapid heart rate, which can reduce the heart’s ability to pump blood effectively. AFib can be classified into three main types:
Paroxysmal AFib: Episodes come and go, usually resolving on their own within 48 hours.
Persistent AFib: Episodes last longer than seven days and require medical intervention to restore normal rhythm.
Permanent AFib: Continuous irregular rhythm that cannot be restored to normal despite treatment.
See Also: What Are The Signs of Arrhythmia
Symptoms And Diagnosis
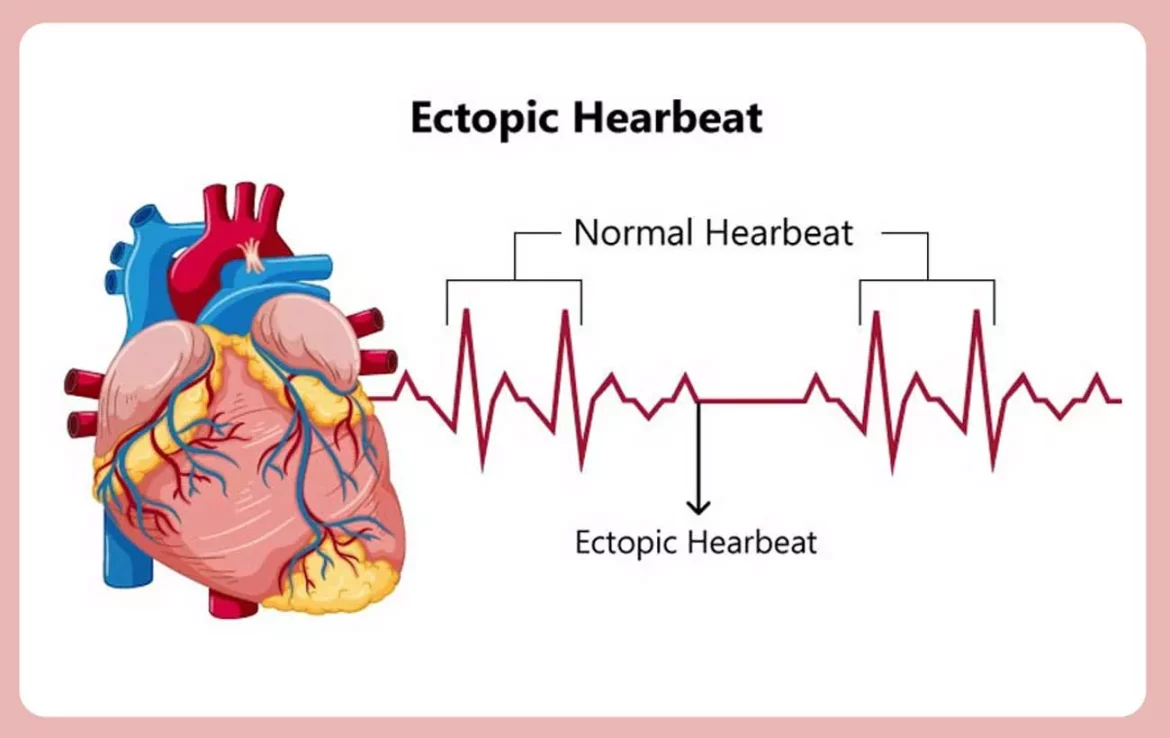
Common symptoms of AFib include palpitations, shortness of breath, fatigue, chest pain, and dizziness. Diagnosis typically involves:
Electrocardiogram (ECG): The primary tool for detecting AFib.
Holter Monitor: A portable ECG device worn for 24-48 hours to monitor heart activity.
Echocardiogram: An ultrasound of the heart to assess its structure and function.
Blood Tests: To check for underlying conditions like thyroid disease.
Stress Test: To evaluate heart function during physical activity.
Comprehensive Management of Atrial Fibrillation
Effective treatment of AFib involves a multifaceted approach aimed at restoring normal heart rhythm, controlling heart rate, preventing stroke, and addressing underlying causes. The following are key components of AFib management:
- Medications
- Non-Pharmacological Treatments
- Lifestyle Modifications
- Monitoring and Follow-Up
What to Give for AFib
Medications play a pivotal role in managing AFib, categorized into rate control, rhythm control, and anticoagulation.
Rate Control Medications
Rate control is essential to prevent the heart from beating too quickly. Medications used include:
Beta-Blockers: Drugs like metoprolol, atenolol, and propranolol slow the heart rate by blocking the effects of adrenaline.
Calcium Channel Blockers: Diltiazem and verapamil help slow the heart rate by blocking calcium channels in the heart.
Digoxin: An older medication that can be effective, particularly in patients with heart failure.
Rhythm Control Medications
Rhythm control aims to restore and maintain normal heart rhythm (sinus rhythm). These medications include:
Antiarrhythmic Drugs: Amiodarone, sotalol, and flecainide help maintain normal rhythm. Amiodarone is particularly effective but has potential long-term side effects.
Sodium Channel Blockers: Propafenone and quinidine help stabilize the heart’s electrical activity.
Anticoagulation Medications
AFib significantly increases the risk of stroke due to the formation of blood clots in the atria. Anticoagulants, also known as blood thinners, are essential to reduce this risk:
Warfarin: A traditional anticoagulant requiring regular blood monitoring to ensure proper dosing.
Direct Oral Anticoagulants (DOACs): Including dabigatran, rivaroxaban, apixaban, and edoxaban. These newer agents do not require frequent monitoring and have fewer dietary restrictions.
see also: Why Does Afib Cause Chest Pain
Additional Medications
Depending on the patient’s condition, additional medications may be necessary:
Diuretics: To reduce fluid buildup in patients with heart failure.
ACE Inhibitors and ARBs: To manage hypertension and heart failure, contributing to overall cardiovascular health.
Non-Pharmacological Treatments
In some cases, medications alone may not be sufficient to control AFib, necessitating non-pharmacological interventions.
Electrical Cardioversion
A procedure that uses electrical shocks to reset the heart’s rhythm. It is often performed under sedation and is effective in restoring normal rhythm in many patients.
Catheter Ablation
A minimally invasive procedure where catheters are inserted through the blood vessels to the heart to destroy (ablate) the tissue causing the abnormal signals. This technique is particularly useful for patients with persistent or difficult-to-control AFib.
Surgical Interventions
For patients who do not respond to other treatments, surgical options like the Maze procedure may be considered. This involves creating a series of incisions in the atria to disrupt the erratic electrical pathways.
Lifestyle Modifications
Lifestyle changes are a critical component of managing AFib and improving overall cardiovascular health.
Diet and Nutrition
Heart-Healthy Diet: Emphasizing fruits, vegetables, whole grains, lean proteins, and healthy fats.
Reduce Sodium Intake: To manage blood pressure and fluid retention.
Limit Alcohol and Caffeine: Both can trigger AFib episodes.
Physical Activity
Regular exercise is important, but it should be moderate and tailored to the individual’s fitness level. Activities like walking, swimming, and cycling are recommended.
Weight Management
Maintaining a healthy weight is crucial, as obesity is a risk factor for AFib. Weight loss can significantly improve AFib symptoms and outcomes.
Stress Management
Stress can exacerbate AFib. Techniques such as yoga, meditation, and deep breathing exercises can help manage stress levels.
Monitoring And Follow-Up
Regular follow-up with healthcare providers is essential to monitor the effectiveness of treatment, adjust medications, and detect any complications early.
Self-Monitoring
Patients are often encouraged to monitor their heart rate and rhythm at home using wearable devices or apps. Keeping a symptom diary can also help in managing AFib.
Regular Check-Ups
Routine visits to the cardiologist ensure that treatment plans are optimized and any new symptoms or side effects are promptly addressed.
Conclusion
Atrial fibrillation is a complex condition requiring a comprehensive treatment approach tailored to each patient. What to give for AFib depends on various factors, including the type of AFib, underlying conditions, and patient preferences.
Medications, non-pharmacological treatments, lifestyle modifications, and regular monitoring all play vital roles in managing AFib effectively. By working closely with healthcare providers, patients can achieve better control of their condition and reduce the risk of complications, leading to improved quality of life.