Left-sided heart failure, a condition where the left ventricle of the heart cannot pump blood effectively, is a significant health concern due to its prevalence and impact on morbidity and mortality. Understanding the pathophysiology of left-sided heart failure is crucial for developing effective treatments and improving patient outcomes. This article delves into the underlying mechanisms, contributing factors, and physiological changes associated with left-sided heart failure.
What Is The Pathophysiology of Left Sided Heart Failure?
Heart Failure with Reduced Ejection Fraction (HFrEF)
HFrEF, formerly known as systolic heart failure, is characterized by the heart’s inability to contract effectively. This results in a decreased ejection fraction (EF), which is the percentage of blood pumped out of the left ventricle with each heartbeat.
In HFrEF, the EF is typically less than 40%.
Myocardial Infarction and Ischemia
Coronary artery disease is the leading cause of HFrEF. When a myocardial infarction (heart attack) occurs, part of the heart muscle is damaged and replaced with scar tissue, which cannot contract. This reduces the overall contractility of the heart.
Chronic ischemia (reduced blood flow) due to coronary artery disease leads to myocardial stunning and hibernation, where the heart muscle temporarily loses its contractile function.
See Also: The Best SGLT2 Inhibitors for The Treatment of Heart Failure
Cardiomyopathy
Dilated cardiomyopathy is a condition where the heart becomes enlarged and cannot pump blood efficiently. The causes can be genetic, viral, or idiopathic (unknown).
Toxic cardiomyopathy results from exposure to certain toxins or drugs, such as alcohol, cocaine, or chemotherapy agents.
Hypertension
Long-standing hypertension increases the workload on the left ventricle, leading to hypertrophy (thickening) of the ventricular wall.
Over time, the hypertrophied heart muscle becomes less efficient, leading to reduced contractility.
Heart Failure with Preserved Ejection Fraction (HFpEF)
HFpEF, formerly known as diastolic heart failure, occurs when the left ventricle loses its ability to relax properly. This leads to impaired filling of the heart during diastole (the phase of the heartbeat when the heart muscle relaxes and allows the chambers to fill with blood). Despite a normal or near-normal ejection fraction (typically 50% or higher), the heart cannot fill with enough blood, leading to symptoms of heart failure.
Underlying Mechanisms
Hypertension
Systemic hypertension is a major cause of HFpEF. Chronic high blood pressure leads to left ventricular hypertrophy, reducing the ventricle’s ability to relax and fill properly.
Aging
As individuals age, the heart’s compliance (ability to stretch) decreases. This natural process can contribute to HFpEF, especially when combined with other risk factors like hypertension and diabetes.
Obesity and Metabolic Syndrome
Obesity and metabolic syndrome (a cluster of conditions including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels) are increasingly recognized as important contributors to HFpEF.
Diabetes Mellitus
Diabetes can lead to myocardial fibrosis (scarring of the heart tissue) and microvascular dysfunction (small blood vessel abnormalities), both of which impair diastolic function.
Neurohormonal Activation in Heart Failure
Neurohormonal activation plays a crucial role in the pathophysiology of heart failure. When the heart’s pumping capacity is compromised, the body activates various compensatory mechanisms to maintain cardiac output and blood pressure. These mechanisms include the sympathetic nervous system (SNS), the renin-angiotensin-aldosterone system (RAAS), and the release of antidiuretic hormone (ADH).
Sympathetic Nervous System (SNS)
The SNS is activated early in heart failure to increase heart rate and contractility. However, chronic SNS activation leads to detrimental effects, including increased myocardial oxygen demand, arrhythmias, and further myocardial damage.
Renin-Angiotensin-Aldosterone System (RAAS)
The RAAS is activated in response to decreased renal perfusion (blood flow to the kidneys) and sympathetic stimulation.
This system increases blood volume and blood pressure through vasoconstriction (narrowing of blood vessels) and sodium and water retention. Chronic RAAS activation leads to fluid overload, increased cardiac workload, and myocardial remodeling (structural changes in the heart muscle).
Antidiuretic Hormone (ADH)
ADH, also known as vasopressin, is released in response to decreased blood volume and increased plasma osmolality (concentration of solutes in the blood). It promotes water reabsorption in the kidneys, contributing to fluid retention and increased blood volume.
Hemodynamic Changes in Left-Sided Heart Failure
The hemodynamic changes in left-sided heart failure are characterized by increased pressure and volume in the left ventricle and atrium. This leads to a cascade of events affecting the entire cardiovascular system.
Increased Left Ventricular End-Diastolic Pressure (LVEDP)
In both HFrEF and HFpEF, the left ventricle is unable to pump blood effectively, resulting in increased LVEDP. This pressure is transmitted backward to the left atrium and pulmonary veins, leading to pulmonary congestion and edema (fluid accumulation in the lungs).
Pulmonary Hypertension
Chronic elevation of pulmonary venous pressure due to left-sided heart failure leads to pulmonary hypertension (increased pressure in the pulmonary arteries). This condition can cause right-sided heart failure (cor pulmonale) if left untreated.
Reduced Cardiac Output
The impaired pumping ability of the left ventricle leads to reduced cardiac output (the amount of blood the heart pumps per minute). This results in decreased perfusion of vital organs, leading to symptoms such as fatigue, weakness, and exercise intolerance.
Systemic Vascular Resistance
As cardiac output decreases, systemic vascular resistance (the resistance the heart must overcome to pump blood through the systemic circulation) increases due to compensatory vasoconstriction. This further increases the workload on the left ventricle.
Clinical Manifestations of Left-Sided Heart Failure
The clinical manifestations of left-sided heart failure are primarily due to pulmonary congestion and reduced cardiac output.
Pulmonary Congestion
Dyspnea (Shortness of Breath)
Dyspnea is a hallmark symptom of left-sided heart failure. It may occur during exertion (exertional dyspnea), at rest (resting dyspnea), or when lying flat (orthopnea). Paroxysmal nocturnal dyspnea (PND) is a sudden onset of breathlessness during sleep, causing the patient to wake up gasping for air.
Cough and Wheezing
A persistent cough, often worse at night, and wheezing can occur due to fluid accumulation in the lungs.
Pulmonary Edema
Severe fluid accumulation in the lungs can lead to pulmonary edema, characterized by extreme shortness of breath, frothy pink sputum, and crackles (abnormal lung sounds) on auscultation.
Reduced Cardiac Output
Fatigue and Weakness
Reduced perfusion of skeletal muscles leads to fatigue and generalized weakness, particularly during physical activity.
Confusion and Memory Impairment
Decreased cerebral perfusion can cause confusion, memory impairment, and difficulty concentrating.
Decreased Urine Output
Reduced renal perfusion leads to decreased urine output (oliguria) and fluid retention.
Cool, Clammy Skin
Peripheral vasoconstriction in response to reduced cardiac output can cause cool, clammy skin and delayed capillary refill.
Complications of Left-Sided Heart Failure
Left-sided heart failure can lead to numerous complications if not managed effectively.
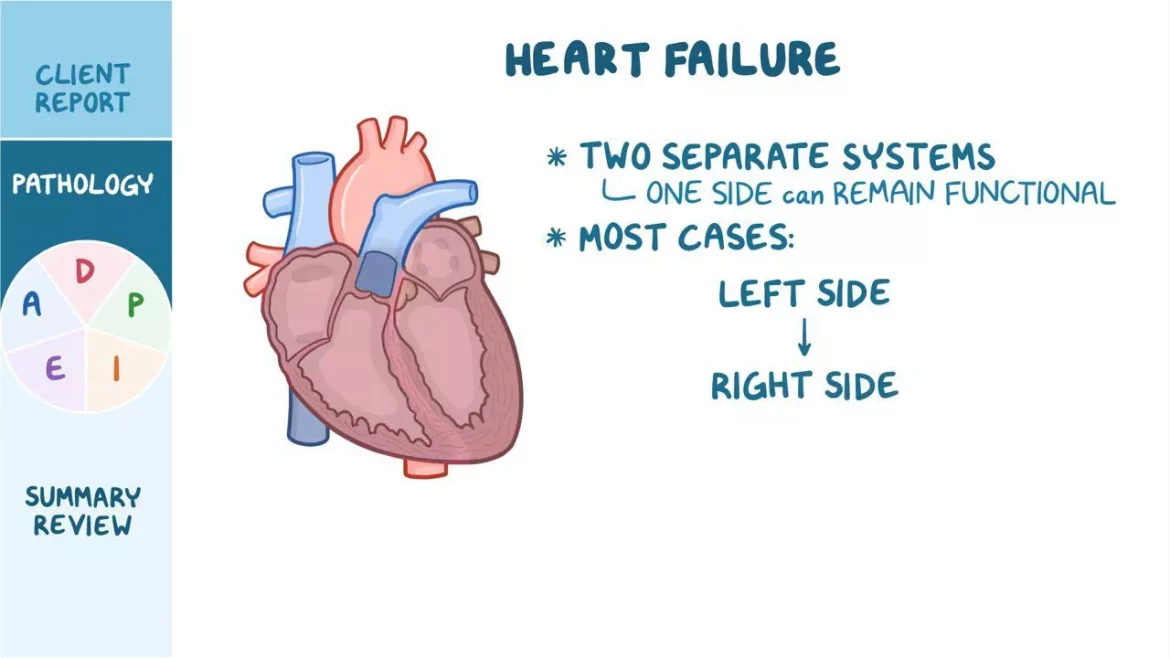
Right-Sided Heart Failure
Chronic left-sided heart failure can cause pulmonary hypertension, leading to right-sided heart failure as the right ventricle struggles to pump blood against the increased pressure in the pulmonary circulation.
Arrhythmias
The structural and electrical remodeling of the heart in heart failure can lead to various arrhythmias, including atrial fibrillation (AF), ventricular tachycardia (VT), and sudden cardiac death (SCD).
Renal Dysfunction
Reduced renal perfusion and the effects of neurohormonal activation can lead to chronic kidney disease (CKD) and acute kidney injury (AKI).
Liver Congestion
Increased central venous pressure in advanced heart failure can cause liver congestion and, eventually, cardiac cirrhosis (fibrosis of the liver due to chronic heart failure).
Surgical Interventions
Coronary Artery Bypass Grafting (CABG)
CABG is performed in patients with significant coronary artery disease to improve blood flow to the heart muscle.
Valve Repair or Replacement
Surgical or transcatheter procedures may be necessary for patients with severe valvular heart disease contributing to heart failure.
Implantable Cardioverter-Defibrillators (ICDs)
ICDs are used in patients at high risk of sudden cardiac death due to arrhythmias. These devices can detect and treat life-threatening arrhythmias.
Left Ventricular Assist Devices (LVADs)
LVADs are mechanical pumps that help the left ventricle pump blood to the rest of the body. They are used in patients with end-stage heart failure as a bridge to transplantation or as destination therapy.
Heart Transplantation
Heart transplantation is considered for patients with refractory heart failure who do not respond to other treatments.
Conclusion
Understanding the pathophysiology of left-sided heart failure is essential for the effective management and treatment of this complex condition. It involves a combination of hemodynamic changes, neurohormonal activation, and structural and functional alterations of the heart. By addressing the underlying causes and implementing appropriate therapeutic strategies, healthcare providers can improve patient outcomes and quality of life.