Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to symptoms such as wheezing, shortness of breath, coughing, and chest tightness. While the primary focus of asthma management is often on controlling respiratory symptoms, it’s important to recognize that asthma can also have systemic effects, including its impact on blood pressure. One of the lesser-known but significant complications of asthma is hypotension, or low blood pressure. In this article, we’ll explore the mechanisms behind why asthma can cause hypotension and the implications of this phenomenon for individuals with asthma.
Understanding Asthma And Its Effects on The Body
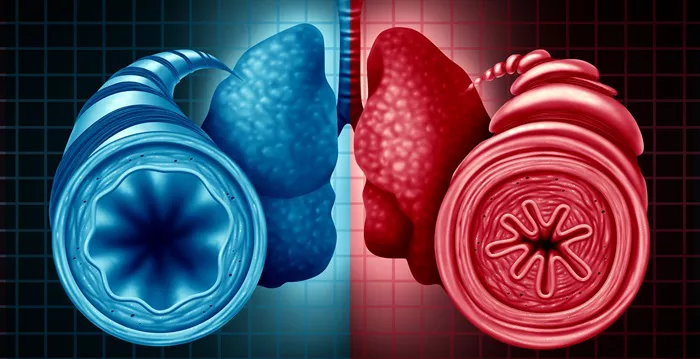
Before delving into the relationship between asthma and hypotension, let’s first understand the basics of asthma and how it affects the body. Asthma is primarily an inflammatory condition of the airways, commonly triggered by allergens, irritants, exercise, or respiratory infections. When a person with asthma encounters a trigger, their airways become inflamed, leading to swelling and narrowing of the passages that carry air to and from the lungs.
This narrowing of the airways results in the characteristic symptoms of asthma, including difficulty breathing, coughing, wheezing, and chest tightness. These symptoms can range from mild to severe and can significantly impact an individual’s quality of life, especially during asthma exacerbations or attacks.
SEE ALSO: Which Seeds Are Good for High Blood Pressure
The Link Between Asthma And Blood Pressure
While asthma is primarily considered a respiratory disorder, its effects can extend beyond the lungs. Research has shown a complex interplay between asthma and cardiovascular function, including the regulation of blood pressure. Hypotension, or low blood pressure, is a condition characterized by a blood pressure reading that is lower than normal, typically defined as a systolic pressure less than 90 mm Hg or a diastolic pressure less than 60 mm Hg.
Why Does Asthma Cause Hypotension?
Respiratory Distress and Hyperventilation: During an asthma attack or when experiencing significant respiratory distress, individuals may engage in rapid, shallow breathing, known as hyperventilation. This rapid breathing can lead to a decrease in carbon dioxide (CO2) levels in the blood, a condition known as respiratory alkalosis. Respiratory alkalosis can affect blood vessel tone and contribute to a drop in blood pressure.
Medication Side Effects: Some medications commonly used to treat asthma, such as beta-agonists (e.g., albuterol) and corticosteroids, can have cardiovascular effects. Beta-agonists can cause vasodilation, leading to a decrease in peripheral vascular resistance and potentially lowering blood pressure. Corticosteroids, especially when used in high doses or for prolonged periods, may also affect blood pressure regulation.
Autonomic Nervous System Dysfunction: Asthma is associated with alterations in autonomic nervous system function, which plays a crucial role in regulating heart rate, blood vessel tone, and blood pressure. Dysregulation of the autonomic nervous system in asthma may contribute to fluctuations in blood pressure, including episodes of hypotension.
Hypoxia: Severe asthma attacks can result in significant hypoxia, or low oxygen levels in the blood. Hypoxia can trigger a cascade of physiological responses, including increased heart rate and peripheral vasodilation, in an attempt to improve oxygen delivery to tissues. However, these compensatory mechanisms can also lead to a drop in blood pressure.
Clinical Implications And Management Strategies
The presence of hypotension in individuals with asthma can have several clinical implications and may require specialized management strategies:
Monitoring: Healthcare providers should monitor blood pressure regularly in individuals with asthma, especially during acute exacerbations or when adjusting medication regimens. Monitoring can help identify and manage hypotension early.
Medication Selection: When prescribing medications for asthma management, healthcare providers should consider the potential cardiovascular effects, including their impact on blood pressure. It may be necessary to adjust medication doses or consider alternative agents in individuals with known hypotension.
Fluid Management: Adequate fluid intake is essential for maintaining blood pressure stability. Individuals with asthma should be encouraged to stay hydrated, especially during periods of increased respiratory symptoms or when using medications that may contribute to fluid loss.
Risk Assessment: Healthcare providers should assess the overall cardiovascular risk profile of individuals with asthma, taking into account factors such as age, comorbidities (e.g., hypertension), and medication history. This holistic approach can help identify and address potential cardiovascular complications, including hypotension.
Education and Awareness: Patients with asthma should receive education about the potential cardiovascular effects of their condition and medications. Empowering patients to recognize signs of hypotension, such as dizziness, lightheadedness, or fainting, can facilitate early intervention and prevent complications.
Conclution
In conclusion, asthma can have systemic effects beyond the respiratory system, including its impact on blood pressure regulation. Hypotension, or low blood pressure, can occur in individuals with asthma due to various factors, including respiratory distress, medication side effects, autonomic nervous system dysfunction, and hypoxia. Healthcare providers should be vigilant in monitoring blood pressure, selecting appropriate medications, managing fluid balance, assessing cardiovascular risk, and educating patients to optimize the management of asthma-related hypotension.