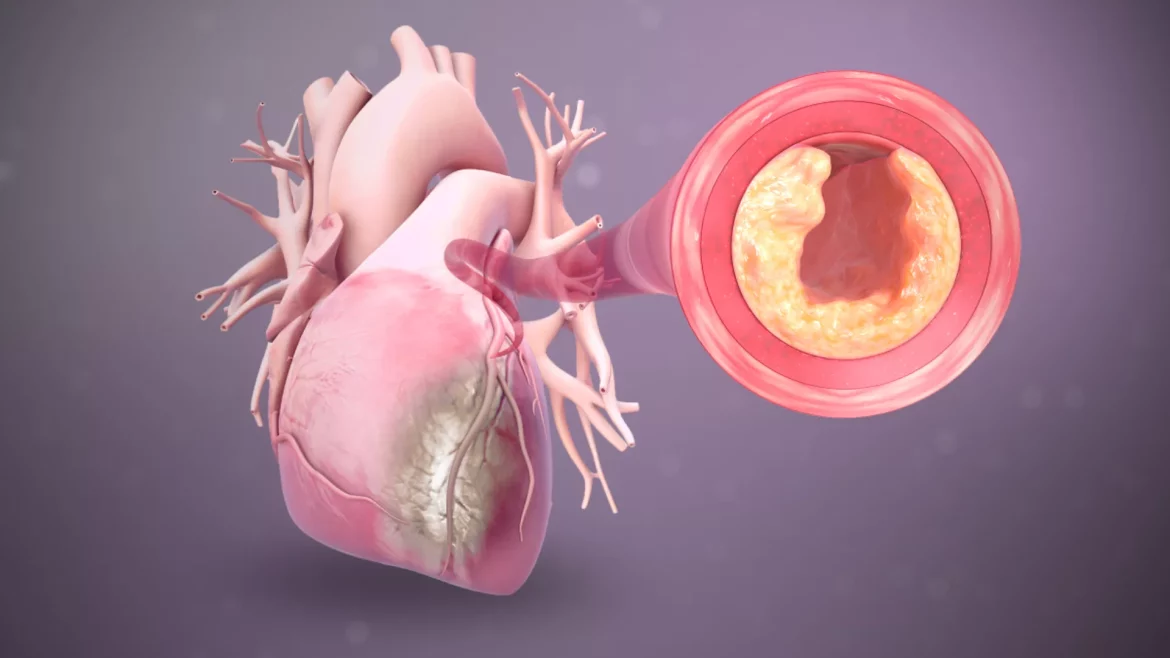
Heart inflammation, or myocarditis, involves inflammation of the heart muscle, and can also refer to inflammation of the surrounding structures such as the pericardium in pericarditis. Testing and diagnosing heart inflammation is critical as it can affect heart function and lead to more severe health issues, including heart failure, arrhythmias, and sudden cardiac death if left untreated. This article provides a detailed guide on how to approach testing for heart inflammation, the types of tests used, their interpretation, and an overview of the underlying pathophysiology.
Understanding Heart Inflammation
Heart inflammation can arise from various causes, with the most common being viral infections. Other causes include bacterial infections, autoimmune diseases, and the side effects of certain medications. Clinically, it presents with a range of symptoms such as chest pain, palpitations, shortness of breath, or fatigue, and can mimic many other heart conditions, making accurate diagnosis vital yet challenging.
SEE ALSO: how do you get a virus in your heart
Types of Heart Inflammation
Myocarditis: This primarily involves the myocardium or the heart muscle. It can lead to dilated cardiomyopathy if chronic.
Pericarditis: This is the inflammation of the pericardium, a fluid-filled sac surrounding the heart.
Endocarditis: Although more of an infection than inflammation, it involves the inner lining of the heart chambers and heart valves.
How to Test for Heart Hnflammation
Diagnosing heart inflammation typically involves a combination of patient history, clinical examination, and a variety of diagnostic tests.
Given the complex nature of the condition, the diagnostic process is aimed at both confirming the presence of inflammation and determining the underlying cause.
1. Clinical History and Examination
A thorough clinical history is crucial. Physicians will look for symptoms suggestive of heart inflammation, recent infections, medication history, and autoimmune disorders. During physical examination, doctors may look for signs of fluid retention, irregular heartbeats, and heart murmurs.
2. Diagnostic Testing
A range of tests is available to assess heart inflammation:
3. Blood Tests
Troponin T and I: These markers of myocardial injury are elevated in myocarditis and can indicate cardiac damage.
C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR): General markers of inflammation that can be elevated in myocarditis and pericarditis.
Other biomarkers: Specific viruses or autoimmune markers can also be identified through blood tests depending on the suspected etiology.
4. Electrocardiogram (ECG)
An ECG can show abnormalities typical of myocarditis or pericarditis, such as ST segment changes, T wave inversions, or abnormal Q waves.
5. Echocardiogram
This ultrasound examination of the heart provides images that can show areas of poor heart muscle function, fluid around the heart (pericardial effusion), or heart enlargement.
6. Cardiac MRI
Considered the gold standard for diagnosing myocarditis, cardiac MRI can detect changes in the heart muscle indicative of inflammation with high sensitivity and specificity.
7. Endomyocardial Biopsy (EMB)
Though invasive, an EMB can confirm myocarditis by showing inflammatory cells infiltrating the heart muscle. This test is usually reserved for cases where the diagnosis is unclear or treatment has not led to improvement.
Interpreting Test Results
Interpreting the results of these tests involves a holistic consideration of both clinical presentation and diagnostic data:
Elevated biomarkers alone cannot confirm heart inflammation but, combined with symptoms and imaging findings, support the diagnosis.
An ECG and echocardiogram help in the initial assessment but might not be definitive for myocarditis.
Cardiac MRI provides a detailed picture of heart tissue health and is crucial in confirming the diagnosis.
Challenges in Diagnosing Heart Inflammation
The main challenges in diagnosing heart inflammation include its nonspecific symptoms and the varying nature of test results based on the stage of the disease and underlying cause. Moreover, some tests have a risk of false positives or negatives, which necessitates careful interpretation in the clinical context.
Treatment And Management
While specific treatments depend on the underlying cause, general approaches include managing symptoms, preventing complications, and addressing the root cause:
Medications: These might include anti-inflammatory drugs, antibiotics, or antivirals, depending on the cause.
Lifestyle adjustments: Rest and limiting physical activity can be crucial in cases of myocarditis.
Regular monitoring: Follow-up tests such as echocardiograms or MRIs may be necessary to assess recovery or progression of the disease.
Conclusion
Testing for heart inflammation requires a systematic approach involving an array of diagnostic tools. Each test provides critical information that, when combined with clinical expertise, guides effective management. As research evolves, further advancements in diagnostic methodologies are expected, which will enhance our ability to effectively diagnose and treat heart inflammation, thereby improving outcomes for affected patients.