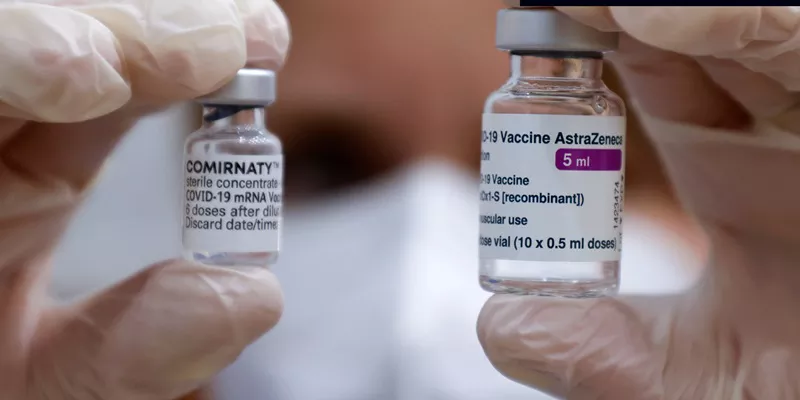
The COVID-19 pandemic has prompted an unprecedented global vaccination effort, with various vaccines being developed, approved, and distributed at a rapid pace. Among these vaccines is the AstraZeneca COVID-19 vaccine, also known as Vaxzevria, which has been widely used in numerous countries. While the vaccine has proven effective in preventing COVID-19, concerns have arisen about potential side effects, including myocarditis, a condition characterized by inflammation of the heart muscle. This article explores the evidence and research surrounding the question: does the AstraZeneca vaccine cause myocarditis?
Understanding Myocarditis
Myocarditis is an inflammatory condition of the heart muscle (myocardium). It can be caused by various factors, including viral infections, autoimmune diseases, and exposure to certain toxins. Symptoms of myocarditis can range from mild, such as fatigue and chest pain, to severe, including heart failure and sudden death. Diagnosis typically involves clinical evaluation, electrocardiograms (ECGs), blood tests, and imaging studies like echocardiography or magnetic resonance imaging (MRI).
SEE ALSO: How Do You Get A Virus in Your Heart
COVID-19 Vaccines And Myocarditis: An Overview
Since the rollout of COVID-19 vaccines, including mRNA vaccines (Pfizer-BioNTech and Moderna) and viral vector vaccines (AstraZeneca and Johnson & Johnson), there have been reports of myocarditis occurring post-vaccination. These reports have primarily focused on mRNA vaccines, which have shown a small but increased risk of myocarditis, particularly in younger males. However, concerns about myocarditis following AstraZeneca vaccination have also emerged, prompting further investigation.
Examining The Evidence: AstraZeneca And Myocarditis
Clinical Trial Data and Initial Reports
During the initial clinical trials of the AstraZeneca vaccine, no significant increase in myocarditis cases was observed compared to the general population. The trials involved tens of thousands of participants, and the safety data did not indicate myocarditis as a common adverse event. However, post-marketing surveillance and real-world data collection are essential for identifying rare side effects that may not appear in clinical trials.
Post-Marketing Surveillance and Case Reports
Since the vaccine’s approval and widespread use, several countries have conducted post-marketing surveillance to monitor adverse events. Reports of myocarditis following AstraZeneca vaccination have been relatively rare compared to the millions of doses administered. In the United Kingdom, where the AstraZeneca vaccine has been widely used, the Medicines and Healthcare products Regulatory Agency (MHRA) has not identified a significant increase in myocarditis cases directly linked to the vaccine.
Comparative Studies and Risk Assessment
Comparative studies examining the risk of myocarditis among different COVID-19 vaccines have provided valuable insights.
A study published in the journal Nature Medicine analyzed data from over 38 million vaccinated individuals across multiple countries. The study found that the risk of myocarditis was higher following mRNA vaccination, particularly in younger males, while the risk associated with viral vector vaccines like AstraZeneca was not significantly elevated. These findings suggest that while myocarditis can occur post-vaccination, the AstraZeneca vaccine does not appear to carry the same level of risk as mRNA vaccines.
MechanismsAnd Pathophysiology
Immune Response and Inflammation
The exact mechanisms by which COVID-19 vaccines might cause myocarditis are not fully understood, but several hypotheses have been proposed. One theory suggests that the immune response triggered by the vaccine may, in rare cases, lead to an overactive inflammatory reaction in the heart. This immune-mediated inflammation could result in myocarditis, particularly in individuals with a predisposition to autoimmune conditions or other risk factors.
Molecular Mimicry
Another potential mechanism is molecular mimicry, where components of the vaccine resemble proteins found in heart tissue, leading the immune system to mistakenly attack the heart. However, evidence supporting this theory is limited, and further research is needed to determine its relevance to vaccine-induced myocarditis.
Temporal Association Vs. Causation
Evaluating Temporal Patterns
Establishing a causal relationship between the AstraZeneca vaccine and myocarditis requires careful evaluation of temporal patterns. Reports of myocarditis typically emerge within days to weeks after vaccination, suggesting a temporal association.
However, distinguishing between coincidental occurrences and true vaccine-induced cases is challenging, especially given the background incidence of myocarditis in the general population.
Investigating Underlying Conditions
It is also important to consider the role of underlying health conditions and individual susceptibility. Some individuals may have pre-existing conditions that predispose them to myocarditis, and these conditions could be exacerbated by vaccination. Detailed medical histories and thorough investigations are necessary to identify such cases and understand their implications.
Regulatory Responses And Recommendations
Regulatory Agency Reviews
Regulatory agencies, including the European Medicines Agency (EMA) and the World Health Organization (WHO), have conducted thorough reviews of the safety data related to the AstraZeneca vaccine. These reviews have concluded that the benefits of vaccination outweigh the risks, including the potential risk of myocarditis. The agencies continue to monitor adverse events and update their recommendations as new data emerge.
Vaccination Recommendations
In light of the available evidence, health authorities have maintained their recommendations for the use of the AstraZeneca vaccine, particularly in populations where the benefits of preventing COVID-19 outweigh the risks of rare adverse events.
For individuals with a history of myocarditis or other severe cardiac conditions, healthcare providers may consider alternative vaccines or additional precautions.
Conclusion
The question of whether the AstraZeneca vaccine causes myocarditis is complex and multifaceted. While rare cases of myocarditis have been reported following AstraZeneca vaccination, the evidence suggests that the risk is lower compared to mRNA vaccines. The overall incidence of myocarditis remains low, and the benefits of vaccination in preventing COVID-19, including severe illness and death, far outweigh the potential risks.
Ongoing surveillance, research, and transparent communication are essential to ensuring public trust and safety.
Healthcare providers and regulatory agencies play a critical role in monitoring vaccine safety, investigating reported cases, and providing evidence-based guidance to the public. As the global vaccination effort continues, understanding and mitigating rare adverse events like myocarditis will remain a priority to safeguard public health.