Paroxysmal atrial fibrillation (PAF) is a type of irregular heart rhythm that begins suddenly and ends on its own within a week, often within 48 hours. Unlike chronic or persistent atrial fibrillation (AF), PAF episodes are self-terminating. However, they can be recurrent, leading to symptoms that can significantly impact a patient’s quality of life. This article delves into the various types of paroxysmal atrial fibrillation, exploring their characteristics, causes, symptoms, and management strategies.
What Is Paroxysmal Atrial Fibrillation?
Paroxysmal atrial fibrillation is a form of AF where episodes of irregular heartbeats start and stop spontaneously. These episodes are typically short-lived, lasting less than seven days and often resolving within 48 hours without medical intervention. The frequency and duration of episodes can vary widely among individuals. PAF is considered less severe than persistent or permanent AF, but it still poses significant health risks, including stroke and heart failure.
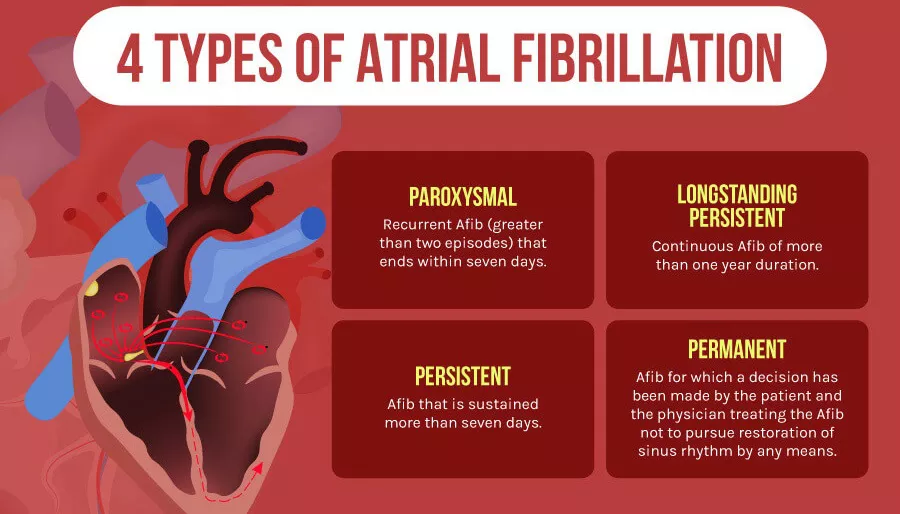
4 Types of Paroxysmal Atrial Fibrillation
While PAF is generally categorized under a single term, it can manifest in various forms, each with unique characteristics and implications for treatment and management. Here are the main types of PAF:
SEE ALSO: What Are Some Home Remedies for Heart Palpitations?
1. Lone Paroxysmal Atrial Fibrillation
Characteristics and Causes
Lone PAF refers to atrial fibrillation occurring in individuals under the age of 60 who have no other heart disease or significant risk factors. The term “lone” implies that the AF is not associated with other cardiovascular conditions, hypertension, or diabetes. The exact cause of lone PAF is often idiopathic, meaning it arises spontaneously without a known reason.
Symptoms and Risks
Patients with lone PAF may experience palpitations, shortness of breath, and fatigue. Despite the lack of underlying heart disease, these episodes can be distressing and disruptive. While the immediate risk of stroke in lone PAF is lower compared to AF associated with structural heart disease, the risk is not zero and should not be ignored.
Management
Management of lone PAF focuses on symptom relief and prevention of thromboembolic events. Treatment options include:
Lifestyle Modifications: Reducing alcohol intake, managing stress, and maintaining a healthy weight.
Medications: Antiarrhythmic drugs, beta-blockers, and anticoagulants if necessary.
Catheter Ablation: In cases where medications are ineffective or not tolerated, catheter ablation may be considered.
2. Secondary Paroxysmal Atrial Fibrillation
Characteristics and Causes
Secondary PAF occurs as a result of an underlying condition or trigger. Common causes include:
Cardiovascular Diseases: Hypertension, coronary artery disease, and heart failure.
Non-Cardiac Triggers: Hyperthyroidism, sleep apnea, and acute infections.
Lifestyle Factors: Excessive alcohol consumption, caffeine intake, and stress.
Symptoms and Risks
Symptoms of secondary PAF are similar to those of lone PAF but may be more severe due to the presence of other health issues. The risk of stroke is higher in secondary PAF due to the associated conditions that increase thromboembolic risk.
Management
The management of secondary PAF involves addressing the underlying cause while managing AF symptoms. Strategies include:
Treating the Underlying Condition: Managing hypertension, treating hyperthyroidism, and addressing sleep apnea.
Medications: Similar to lone PAF, with the addition of specific treatments for the underlying condition.
Lifestyle Modifications: Reducing triggers such as alcohol and caffeine.
3. Symptomatic Paroxysmal Atrial Fibrillation
Characteristics and Causes
Symptomatic PAF is characterized by noticeable and distressing symptoms during AF episodes. These can include palpitations, chest pain, shortness of breath, dizziness, and fatigue. The causes of symptomatic PAF can be diverse and may overlap with those of lone and secondary PAF.
Symptoms and Risks
Patients with symptomatic PAF often experience a significant impact on their quality of life due to the severity and frequency of symptoms.
The risks associated with symptomatic PAF depend on the underlying causes and the patient’s overall health.
Management
Management of symptomatic PAF aims to alleviate symptoms and prevent complications. This includes:
Medications: Antiarrhythmics, beta-blockers, calcium channel blockers, and anticoagulants.
Non-Pharmacological Interventions: Catheter ablation, electrical cardioversion, and lifestyle changes.
Patient Education: Educating patients about symptom management and the importance of medication adherence.
4. Asymptomatic Paroxysmal Atrial Fibrillation
Characteristics and Causes
Asymptomatic PAF, also known as “silent AF,” occurs without noticeable symptoms. It is often detected incidentally during routine medical examinations or through the use of wearable heart monitors.
The causes of asymptomatic PAF are similar to those of other types but may include a higher prevalence of structural heart disease or other comorbid conditions.
Symptoms and Risks
Despite the lack of symptoms, asymptomatic PAF carries the same risks as symptomatic AF, particularly the risk of stroke.
The absence of symptoms can lead to delayed diagnosis and treatment, increasing the potential for complications.
Management
Management strategies for asymptomatic PAF focus on preventing complications and managing underlying conditions.
These include:
Regular Monitoring: Using wearable devices or regular ECGs to detect AF episodes.
Medications: Anticoagulants to prevent stroke, along with other heart medications as needed.
Lifestyle Modifications: Similar to those for other types of PAF, including dietary changes and regular exercise.
Diagnosing Paroxysmal Atrial Fibrillation
Accurate diagnosis of PAF is crucial for effective management.
Diagnostic methods include:
Electrocardiogram (ECG): The primary tool for detecting AF episodes.
Holter Monitor: A portable device worn for 24-48 hours to record heart activity.
Event Monitor: Used for longer periods to capture sporadic AF episodes.
Implantable Loop Recorder: A device implanted under the skin for continuous monitoring over several years.
Risk Factors And Complications
Several risk factors increase the likelihood of developing PAF, including age, hypertension, obesity, diabetes, and a family history of AF. Complications of untreated PAF include:
Stroke: Due to the formation of blood clots in the atria.
Heart Failure: Resulting from prolonged periods of irregular heart rhythms.
Cognitive Decline: Potentially linked to recurrent AF episodes.
Treatment And Management of Paroxysmal Atrial Fibrillation
The treatment approach for PAF depends on the frequency and severity of episodes, underlying causes, and patient preferences. Key components of treatment include:
Medications
Rate Control: Beta-blockers and calcium channel blockers to control heart rate.
Rhythm Control: Antiarrhythmic drugs to maintain normal heart rhythm.
Anticoagulation: Warfarin, direct oral anticoagulants (DOACs) to prevent stroke.
Non-Pharmacological Interventions
Electrical Cardioversion: A procedure to restore normal heart rhythm using electrical shocks.
Catheter Ablation: A minimally invasive procedure to isolate or destroy areas of heart tissue causing AF.
Surgical Ablation: A more invasive option for patients with severe or refractory AF.
Lifestyle Modifications
Diet and Exercise: Maintaining a healthy weight and engaging in regular physical activity.
Alcohol and Caffeine Reduction: Limiting intake to reduce AF triggers.
Stress Management: Techniques such as yoga, meditation, and deep breathing exercises.
Patient Education and Support
Educating patients about PAF, its symptoms, and the importance of adherence to treatment plans is vital. Support groups and counseling can also help patients cope with the psychological impact of living with PAF.
Conclusion
Paroxysmal atrial fibrillation is a complex condition with various types, each requiring a tailored approach to management.
Understanding the differences between lone, secondary, symptomatic, and asymptomatic PAF is crucial for effective treatment and prevention of complications. Through a combination of medical interventions, lifestyle modifications, and patient education, individuals with PAF can achieve better control over their condition and improve their overall quality of life.