Renal hypertension, also known as renovascular hypertension, is a type of high blood pressure caused by narrowing of the arteries that carry blood to the kidneys. This condition is a significant health concern due to its impact on cardiovascular and kidney health. Understanding the causes of renal hypertension is crucial for effective management and treatment.
Pathophysiology of Renal Hypertension
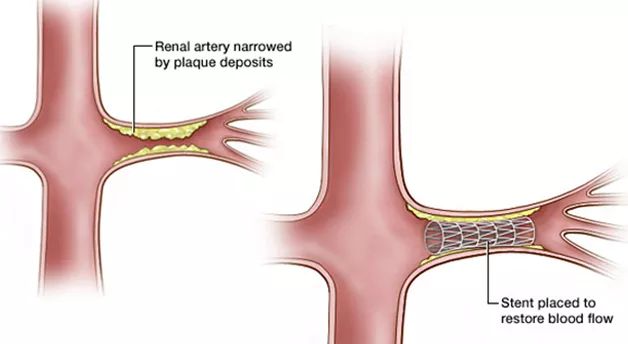
Renal hypertension arises when the arteries supplying the kidneys, known as renal arteries, become narrowed (a condition called renal artery stenosis). This narrowing reduces blood flow to the kidneys. In response to decreased blood flow, the kidneys release hormones that increase blood pressure in an attempt to restore adequate blood flow. This physiological response is beneficial in the short term but can lead to sustained high blood pressure if the underlying issue is not addressed.
SEE ALSO: How OSA Affects Blood Pressure
The Role of The Renin-Angiotensin-Aldosterone System (RAAS)
The kidneys play a critical role in blood pressure regulation through the renin-angiotensin-aldosterone system (RAAS).
When renal blood flow is reduced, the kidneys secrete renin, an enzyme that converts angiotensinogen (produced by the liver) into angiotensin I. Angiotensin I is then converted into angiotensin II by the angiotensin-converting enzyme (ACE) primarily in the lungs. Angiotensin II has several effects that contribute to increased blood pressure:
Vasoconstriction: Angiotensin II causes blood vessels to constrict, increasing vascular resistance and blood pressure.
Aldosterone Secretion: It stimulates the adrenal glands to release aldosterone, which causes the kidneys to retain sodium and water, increasing blood volume and pressure.
Antidiuretic Hormone (ADH) Release: Angiotensin II promotes the release of ADH, which also leads to water retention by the kidneys.
Types of Renal Artery Stenosis
Renal artery stenosis, the primary cause of renal hypertension, can be classified into two main types based on the underlying cause:
Atherosclerotic Renal Artery Stenosis (ARAS)
Atherosclerosis is the most common cause of renal artery stenosis, particularly in older adults. Atherosclerosis is the buildup of fatty plaques within the arterial walls, leading to narrowing and reduced blood flow. Risk factors for atherosclerosis include:
Age: The risk increases with age.
Hypertension: High blood pressure contributes to the development and progression of atherosclerosis.
Hyperlipidemia: Elevated levels of cholesterol and triglycerides promote plaque formation.
Smoking: Smoking damages the endothelium, facilitating plaque development.
Diabetes: Diabetes accelerates atherosclerosis through multiple mechanisms, including oxidative stress and inflammation.
Fibromuscular Dysplasia (FMD)
Fibromuscular dysplasia is a less common cause of renal artery stenosis but is a significant contributor, especially in younger individuals, particularly women. FMD involves abnormal growth of the arterial wall, leading to a beaded appearance and narrowing of the arteries. The exact cause of FMD is unknown, but genetic and hormonal factors are thought to play a role.
Clinical Presentation of Renal Hypertension
Renal hypertension often presents with symptoms typical of high blood pressure, including headaches, dizziness, and visual disturbances. However, it can also lead to more severe complications if left untreated. These complications include:
Chronic Kidney Disease (CKD): Prolonged high blood pressure can damage the kidneys, leading to a decline in their function.
Heart Disease: Renal hypertension increases the risk of heart attacks, heart failure, and other cardiovascular diseases.
Stroke: The increased pressure can lead to cerebrovascular accidents, commonly known as strokes.
Diagnostic Evaluation
The diagnosis of renal hypertension involves several steps, including a thorough medical history, physical examination, and various diagnostic tests. These tests help determine the presence and extent of renal artery stenosis and assess kidney function. Key diagnostic tools include:
Blood Pressure Measurement: Persistent high blood pressure, especially if resistant to standard treatments, may suggest renal hypertension.
Laboratory Tests: Blood tests can evaluate kidney function (e.g., serum creatinine, blood urea nitrogen) and check for electrolyte imbalances.
Imaging Studies: Imaging techniques such as Doppler ultrasound, computed tomography (CT) angiography, and magnetic resonance angiography (MRA) can visualize the renal arteries and detect stenosis.
Renal Angiography: This invasive procedure involves injecting contrast dye into the renal arteries to obtain detailed images and is considered the gold standard for diagnosing renal artery stenosis.
Management And Treatment of Renal Hypertension
Effective management of renal hypertension requires addressing both high blood pressure and the underlying cause of renal artery stenosis.
Treatment options include lifestyle modifications, medications, and interventional procedures.
Lifestyle Modifications
Adopting a healthy lifestyle is crucial for managing hypertension and reducing the risk of complications. Key lifestyle changes include:
Diet: A heart-healthy diet, such as the DASH (Dietary Approaches to Stop Hypertension) diet, can help lower blood pressure. This diet emphasizes fruits, vegetables, whole grains, and low-fat dairy products while reducing sodium, saturated fats, and added sugars.
Exercise: Regular physical activity can help lower blood pressure and improve overall cardiovascular health. Aim for at least 150 minutes of moderate-intensity exercise per week.
Weight Management: Maintaining a healthy weight through diet and exercise can significantly impact blood pressure control.
Smoking Cessation: Quitting smoking is essential to reduce the risk of atherosclerosis and improve overall cardiovascular health.
Alcohol Moderation: Limiting alcohol intake can help control blood pressure. Men should limit their intake to two drinks per day, and women to one drink per day.
Medications
Medications play a central role in managing renal hypertension. Commonly used drugs include:
Angiotensin-Converting Enzyme (ACE) Inhibitors and Angiotensin II Receptor Blockers (ARBs): These medications help relax blood vessels and reduce the effects of the RAAS, lowering blood pressure and protecting kidney function.
Calcium Channel Blockers: These drugs help relax blood vessels and reduce the workload on the heart, lowering blood pressure.
Diuretics: Diuretics help remove excess sodium and water from the body, reducing blood volume and pressure.
Beta-Blockers: These medications reduce the heart rate and the heart’s workload, lowering blood pressure.
Interventional Procedures
In cases where lifestyle changes and medications are insufficient, interventional procedures may be necessary to restore adequate blood flow to the kidneys. These procedures include:
Angioplasty and Stenting: This minimally invasive procedure involves inflating a balloon within the narrowed artery to widen it, followed by placing a stent to keep it open. Angioplasty and stenting are often used for atherosclerotic renal artery stenosis.
Surgical Revascularization: In some cases, especially when angioplasty is not feasible, surgical revascularization may be required. This procedure involves bypassing the narrowed section of the artery using a graft.
Conclusion
Renal hypertension is a complex condition primarily caused by narrowing of the renal arteries, leading to increased blood pressure. Understanding the underlying causes, such as atherosclerosis and fibromuscular dysplasia, is crucial for effective diagnosis and treatment. Management strategies include lifestyle modifications, medications, and interventional procedures, with the goal of controlling blood pressure, restoring adequate blood flow to the kidneys, and preventing complications.