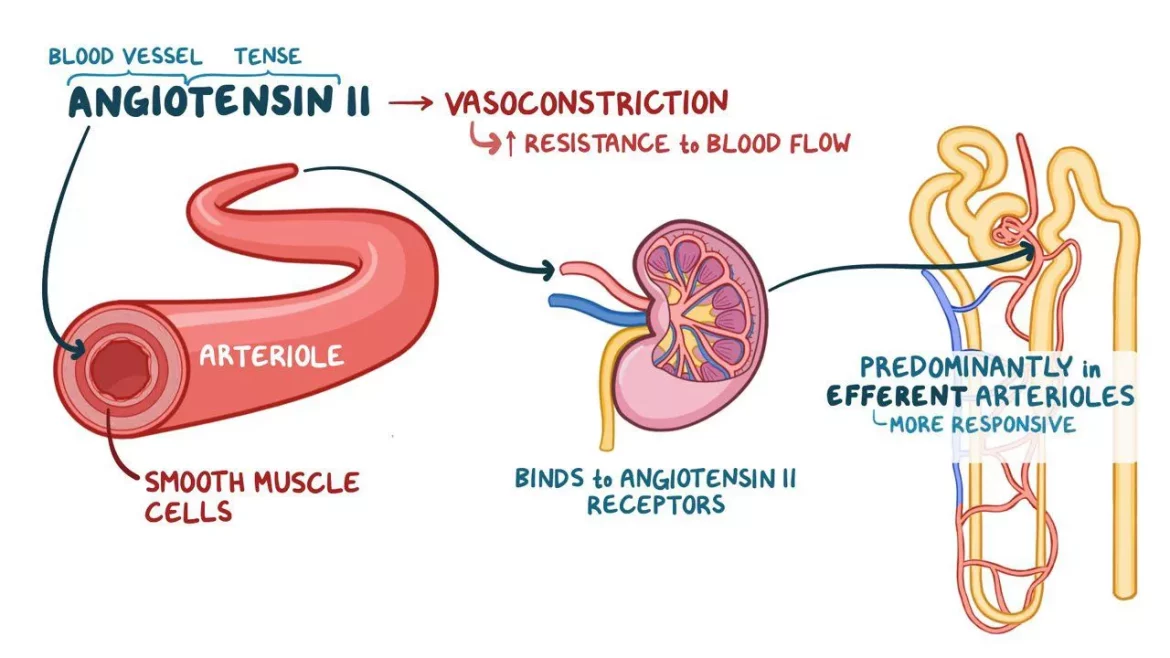
Renin is an enzyme secreted by the kidneys that plays a crucial role in regulating blood pressure, electrolyte balance, and fluid volume in the body. It is a part of the renin-angiotensin-aldosterone system (RAAS), which is vital for maintaining cardiovascular and renal health. When blood pressure drops, the kidneys release renin into the bloodstream. Renin then converts angiotensinogen, a protein produced by the liver, into angiotensin I. Angiotensin I is further converted into angiotensin II by the enzyme angiotensin-converting enzyme (ACE). Angiotensin II constricts blood vessels and stimulates the release of aldosterone from the adrenal glands, which causes the kidneys to retain sodium and water, increasing blood pressure.
Low Renin Levels And Their Implications
Low renin levels, also known as hyporeninemia, can have significant implications for cardiovascular health. Low renin can be a sign of underlying health conditions and can contribute to various forms of heart disease. Understanding the causes of low renin in heart disease is essential for diagnosing and managing these conditions effectively.
SEE ALSO: What Are The Types of Renal Artery Stenosis?
Primary Causes of Low Renin in Heart Disease
Primary Aldosteronism
Primary aldosteronism, also known as Conn’s syndrome, is a condition characterized by the overproduction of aldosterone by the adrenal glands. This excessive aldosterone leads to increased sodium retention, potassium excretion, and water retention, resulting in high blood pressure. In primary aldosteronism, the renin levels are typically low due to the negative feedback mechanism where high blood pressure suppresses renin secretion.
Renal Disease
Chronic kidney disease (CKD) and other forms of renal impairment can lead to low renin levels. The kidneys are responsible for renin production, and any damage or dysfunction in the renal tissue can impair the secretion of renin. In CKD, the kidneys are less able to respond to low blood pressure, leading to a state of relative renin deficiency.
Congenital Adrenal Hyperplasia
Congenital adrenal hyperplasia (CAH) is a group of genetic disorders affecting the adrenal glands’ ability to produce cortisol. One form of CAH, 11-beta-hydroxylase deficiency, can lead to low renin levels. This deficiency causes excessive production of deoxycorticosterone, a potent mineralocorticoid, which suppresses renin secretion.
Diabetic Nephropathy
Diabetic nephropathy, a common complication of diabetes, can also cause low renin levels. High blood sugar levels damage the blood vessels in the kidneys, impairing their ability to produce renin. This condition is often associated with hypertension and other cardiovascular diseases.
Liddle Syndrome
Liddle syndrome is a rare genetic disorder characterized by mutations in the epithelial sodium channel (ENaC) that leads to excessive sodium reabsorption in the kidneys. This sodium retention results in hypertension, low renin levels, and low aldosterone levels. Patients with Liddle syndrome often present with early-onset hypertension and hypokalemia.
Secondary Causes And Contributing Factors
In addition to primary causes, several secondary factors can contribute to low renin levels in heart disease. These factors often exacerbate underlying conditions or influence the renin-angiotensin-aldosterone system (RAAS) in indirect ways.
Medications
Certain medications can influence renin levels. Beta-blockers, commonly prescribed for hypertension and heart disease, can reduce renin secretion by inhibiting the sympathetic nervous system’s influence on the kidneys. Nonsteroidal anti-inflammatory drugs (NSAIDs) can also lower renin levels by inhibiting prostaglandin synthesis, which plays a role in renin release.
Age
Renin levels naturally decline with age. This decline can be more pronounced in individuals with pre-existing cardiovascular conditions. Aging-related changes in renal function and hormonal regulation can contribute to lower renin levels in elderly patients.
Obesity
Obesity is a significant risk factor for hypertension and heart disease. It can also affect renin levels by altering the balance of various hormones and increasing the production of certain adipokines that influence the RAAS. Obesity-related changes in renal hemodynamics can further suppress renin secretion.
Dietary Factors
Diets high in sodium can lead to low renin levels. Excessive sodium intake increases blood pressure, which suppresses renin release through negative feedback mechanisms. Conversely, low potassium intake can also affect renin levels, as potassium is essential for proper renal function and renin secretion.
Hormonal Imbalances
Hormonal imbalances, particularly involving adrenal hormones, can impact renin levels. Conditions such as Cushing’s syndrome, characterized by excess cortisol production, can suppress renin release. Hyperparathyroidism, with elevated parathyroid hormone levels, can also influence renal function and renin secretion.
Clinical Implications And Management
Low renin levels in heart disease can complicate the management of hypertension and other cardiovascular conditions. Identifying the underlying cause of low renin is crucial for effective treatment and management. Here are some clinical implications and management strategies:
Diagnosis
Diagnosing the cause of low renin involves a thorough clinical evaluation, including medical history, physical examination, and laboratory tests. Blood tests to measure renin, aldosterone, and electrolyte levels, along with imaging studies like renal ultrasound or CT scans, can help identify underlying conditions such as primary aldosteronism or renal disease.
Treatment
Treatment strategies for low renin levels depend on the underlying cause. In primary aldosteronism, surgical removal of the adrenal adenoma or medical management with aldosterone antagonists like spironolactone or eplerenone can be effective.
For renal disease, managing blood pressure and controlling blood sugar levels are crucial. In cases of CAH or Liddle syndrome, specific hormonal therapies or potassium-sparing diuretics may be required.
Lifestyle Modifications
Lifestyle modifications can play a significant role in managing low renin levels and associated cardiovascular conditions.
Reducing sodium intake, increasing potassium-rich foods, maintaining a healthy weight, and regular physical activity can help regulate blood pressure and improve overall cardiovascular health.
Monitoring and Follow-up
Regular monitoring of blood pressure, renal function, and electrolyte levels is essential for patients with low renin levels.
Follow-up visits with healthcare providers can help adjust treatment plans and ensure optimal management of underlying conditions.
Conclusion
Low renin levels in heart disease can result from various primary and secondary causes, including primary aldosteronism, renal disease, genetic disorders, and certain medications. Understanding the underlying mechanisms and contributing factors is crucial for effective diagnosis and management. By addressing the root causes and implementing appropriate treatment strategies, healthcare providers can help patients manage their cardiovascular conditions and improve their overall health.