E78 Type 5 hyperlipidemia is a complex metabolic disorder characterized by elevated levels of chylomicrons and very low-density lipoproteins (VLDL) in the blood. This condition is also known as mixed hyperlipidemia or familial combined hyperlipidemia. It is important to understand the underlying mechanisms, clinical implications, and effective treatments to manage this condition efficiently.
Etiology And Pathophysiology
Type 5 hyperlipidemia can be either primary, due to genetic factors, or secondary, caused by other underlying conditions such as diabetes mellitus, obesity, or alcohol abuse. The primary form often results from mutations in genes involved in lipid metabolism, such as the lipoprotein lipase (LPL) gene or the apolipoprotein C-II (ApoC-II) gene. These mutations lead to impaired clearance of chylomicrons and VLDL from the bloodstream, causing their accumulation.
SEE ALSO: How Long Does It Take to Lower Cholesterol with Diet & Exercise
Clinical Manifestations
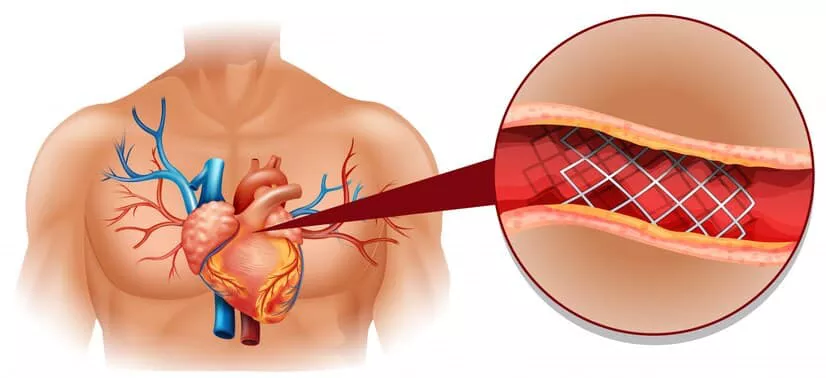
Patients with Type 5 hyperlipidemia often present with xanthomas (fatty deposits under the skin), pancreatitis, and an increased risk of cardiovascular disease. The elevated levels of triglycerides and cholesterol in the blood contribute to the formation of atherosclerotic plaques, which can lead to coronary artery disease, myocardial infarction, and stroke.
Diagnosis
Diagnosis of Type 5 hyperlipidemia involves a combination of clinical assessment, family history, and laboratory investigations. Blood tests reveal elevated triglyceride levels, typically above 1000 mg/dL, and increased cholesterol levels.
Lipoprotein electrophoresis or ultracentrifugation may be used to identify the specific lipoprotein abnormalities.
Treatment Approaches
1. Lifestyle Modifications
Dietary Changes
Diet plays a crucial role in managing Type 5 hyperlipidemia. Patients are advised to adopt a low-fat, low-cholesterol diet.
This includes reducing the intake of saturated fats, trans fats, and cholesterol-rich foods. Increasing dietary fiber through the consumption of fruits, vegetables, whole grains, and legumes can help reduce lipid levels.
Weight Management
Obesity is a significant risk factor for hyperlipidemia. Weight loss through a combination of diet and exercise can substantially improve lipid profiles. Aiming for a gradual weight loss of 1-2 pounds per week is recommended.
Exercise
Regular physical activity helps improve lipid metabolism and reduce triglyceride levels. Patients should aim for at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, cycling, or swimming.
2. Pharmacological Treatment
Fibrates
Fibrates, such as fenofibrate and gemfibrozil, are the primary medications used to treat elevated triglycerides in Type 5 hyperlipidemia. They activate peroxisome proliferator-activated receptors (PPARs), leading to increased lipolysis and clearance of triglyceride-rich particles from the plasma.
Omega-3 Fatty Acids
Omega-3 fatty acids, found in fish oil supplements, have been shown to reduce triglyceride levels. They work by inhibiting the synthesis of triglycerides in the liver and promoting their clearance from the blood.
Nicotinic Acid (Niacin)
Niacin, a B vitamin, is effective in lowering triglycerides and increasing high-density lipoprotein (HDL) cholesterol.
However, its use is limited by side effects such as flushing, gastrointestinal disturbances, and hepatotoxicity.
Statins
While statins are primarily used to lower LDL cholesterol, they can also have a modest effect on reducing triglycerides. In patients with Type 5 hyperlipidemia, statins may be used in combination with other lipid-lowering agents to achieve optimal lipid control.
3. Management of Secondary Causes
Identifying and treating underlying conditions contributing to Type 5 hyperlipidemia is essential. This includes managing diabetes, controlling obesity, reducing alcohol intake, and addressing hypothyroidism. Effective management of these conditions can help reduce lipid levels and improve overall cardiovascular health.
4. Monitoring and Follow-Up
Regular monitoring of lipid levels is crucial to assess the effectiveness of treatment and make necessary adjustments.
Patients should have their lipid profiles checked every 3-6 months. In addition, monitoring for potential side effects of medications is important to ensure patient safety.
Emerging Therapies
Research is ongoing to develop new therapies for hyperlipidemia. Novel agents such as antisense oligonucleotides, gene therapy, and monoclonal antibodies targeting specific pathways in lipid metabolism hold promise for the future.
1. Antisense Oligonucleotides
Antisense oligonucleotides are designed to inhibit the production of specific proteins involved in lipid metabolism. For example, mipomersen targets apolipoprotein B-100, a key component of VLDL and LDL particles, reducing their production and lowering lipid levels.
2. Gene Therapy
Gene therapy aims to correct genetic mutations responsible for hyperlipidemia. Techniques such as CRISPR-Cas9 have the potential to edit faulty genes and restore normal lipid metabolism. Although still in experimental stages, gene therapy could offer a long-term solution for genetic forms of hyperlipidemia.
3. Monoclonal Antibodies
Monoclonal antibodies, such as evolocumab and alirocumab, target proprotein convertase subtilisin/kexin type 9 (PCSK9), a protein that regulates LDL receptor degradation. By inhibiting PCSK9, these antibodies increase LDL receptor availability, enhancing LDL clearance from the bloodstream.
4. Patient Education and Support
Educating patients about the importance of adherence to lifestyle modifications and medications is crucial for successful management of Type 5 hyperlipidemia. Providing resources, support groups, and regular follow-up appointments can help patients stay motivated and informed about their condition.
Conclusion
E78 Type 5 hyperlipidemia is a multifaceted disorder requiring a comprehensive approach to management. Lifestyle modifications, pharmacological treatment, and management of secondary causes are essential components of treatment.
Emerging therapies hold promise for the future, offering new hope for patients with this challenging condition.