Tachycardia is a term that often surfaces in discussions about heart health, yet there can be confusion about its classification and implications. Specifically, whether tachycardia is considered an arrhythmia is a question that merits a thorough exploration. This article delves into the nuances of tachycardia, its relationship to arrhythmias, the underlying mechanisms, types, causes, symptoms, diagnosis, treatment, and management strategies, providing a comprehensive understanding of this cardiovascular condition.
What Is Tachycardia?
Tachycardia refers to a heart rate that exceeds the normal resting rate. Generally, a resting heart rate of more than 100 beats per minute (bpm) in adults is considered tachycardic. The normal resting heart rate for adults ranges from 60 to 100 bpm, though this can vary depending on factors such as age, fitness level, and individual health conditions.
Tachycardia can be categorized based on its origin in the heart: supraventricular (originating above the ventricles) or ventricular (originating in the ventricles).
SEE ALSO: What Is The Cause of Paroxysmal Supraventricular Tachycardia
Is Tachycardia An Arrhythmia?
Tachycardia is indeed considered an arrhythmia. An arrhythmia is any deviation from the normal rhythm of the heart, including irregular, too fast, or too slow heartbeats. Since tachycardia involves an abnormally fast heart rate, it falls under the broader category of arrhythmias.
Arrhythmias encompass a wide range of conditions, from benign and asymptomatic to severe and life-threatening.
Tachycardia can also vary in its clinical significance, depending on its type, duration, and underlying cause.
Types of Tachycardia
Tachycardia can be classified into several types, each with distinct characteristics and implications:
Atrial Tachycardia: This type originates in the atria, the upper chambers of the heart. It is often caused by abnormal electrical signals in the atria and can lead to rapid heart rates.
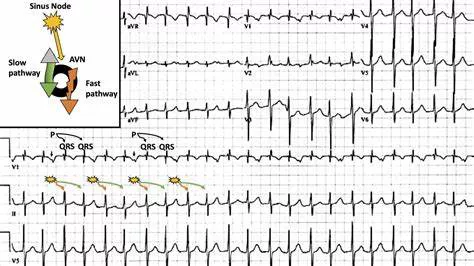
Supraventricular Tachycardia (SVT): SVT is a broad term that encompasses various types of tachycardia originating above the ventricles. It includes atrial tachycardia, atrioventricular nodal reentrant tachycardia (AVNRT), and atrioventricular reciprocating tachycardia (AVRT).
Ventricular Tachycardia (VT): VT originates in the ventricles, the lower chambers of the heart. It can be particularly dangerous and may lead to ventricular fibrillation, a life-threatening condition requiring immediate medical attention.
Sinus Tachycardia: This type originates from the sinus node, the heart’s natural pacemaker. It can be physiological, such as during exercise or stress, or pathological, indicating an underlying condition such as fever, anemia, or hyperthyroidism.
Causes of Tachycardia
The causes of tachycardia are diverse and can be categorized into cardiac and non-cardiac factors:
Cardiac Causes:
- Coronary artery disease
- Heart failure
- Myocardial infarction (heart attack)
- Cardiomyopathy
- Valvular heart disease
- Congenital heart defects
Non-Cardiac Causes:
- Anemia
- Hyperthyroidism
- Fever
- Dehydration
- Electrolyte imbalances
- Alcohol or drug use
- Stress and anxiety
- Certain medications (e.g., stimulants, decongestants)
Symptoms of Tachycardia
The symptoms of tachycardia can vary widely depending on the type and severity of the condition. Common symptoms include:
Palpitations (rapid, pounding, or fluttering heartbeats)
Shortness of breath
Dizziness or lightheadedness
Chest pain or discomfort
Fainting (syncope) or near-fainting spells
Fatigue or weakness
In some cases, especially with brief episodes of tachycardia, individuals may be asymptomatic and the condition might be detected incidentally during a routine examination.
Diagnosis of Tachycardia
Diagnosing tachycardia involves a combination of patient history, physical examination, and diagnostic tests. Key diagnostic tools include:
Electrocardiogram (ECG): This test records the electrical activity of the heart and can identify the type and origin of the tachycardia.
Holter Monitor: A portable device worn for 24-48 hours to continuously monitor the heart’s activity, capturing intermittent episodes of tachycardia.
Event Monitor: Similar to a Holter monitor but worn for a longer period (weeks to months), activated by the patient when symptoms occur.
Echocardiogram: An ultrasound of the heart that provides detailed images of its structure and function, helping to identify underlying heart disease.
Stress Test: A test that assesses the heart’s response to physical exertion, useful in detecting exercise-induced tachycardia.
Electrophysiological Study (EPS): An invasive test that maps the electrical pathways of the heart, often used to pinpoint the origin of tachycardia and guide treatment.
Treatment And Management of Tachycardia
The treatment of tachycardia depends on its type, severity, underlying cause, and the presence of symptoms. Management strategies can be broadly categorized into lifestyle modifications, medications, and interventional procedures:
Lifestyle Modifications:
Avoiding triggers such as caffeine, alcohol, and stimulants
Managing stress through relaxation techniques and counseling
Ensuring adequate hydration and electrolyte balance
Regular physical activity and maintaining a healthy weight
Medications:
Beta-blockers: Reduce heart rate and prevent episodes of tachycardia.
Calcium channel blockers: Help control heart rate and rhythm.
Antiarrhythmic drugs: Used to restore normal heart rhythm and prevent recurrent episodes.
Anticoagulants (blood thinners): Prescribed in cases of atrial tachycardia to prevent stroke.
Interventional Procedures:
Catheter Ablation: A minimally invasive procedure that destroys abnormal electrical pathways causing tachycardia, often curative for many types of SVT and some forms of VT.
Pacemaker: A device implanted to regulate heart rate, used in cases where tachycardia alternates with bradycardia (slow heart rate).
Implantable Cardioverter Defibrillator (ICD): A device that detects and corrects life-threatening ventricular tachycardia and fibrillation by delivering electrical shocks.
Prognosis And Complications
The prognosis of tachycardia varies widely based on its type and underlying cause. Supraventricular tachycardia generally has a good prognosis with appropriate treatment, while ventricular tachycardia, particularly in the presence of structural heart disease, can be more serious and requires careful management.
Potential complications of tachycardia include:
Heart Failure: Prolonged tachycardia can weaken the heart muscle, leading to heart failure.
Stroke: Atrial tachycardia, particularly atrial fibrillation, increases the risk of stroke due to blood clots forming in the atria.
Cardiac Arrest: Untreated or severe ventricular tachycardia can progress to ventricular fibrillation, resulting in cardiac arrest and sudden death.
Conclusion
In summary, tachycardia is indeed considered an arrhythmia, encompassing a range of conditions characterized by an abnormally fast heart rate. Understanding the types, causes, symptoms, diagnostic methods, and treatment options for tachycardia is crucial for effective management and improving patient outcomes. While some forms of tachycardia are benign and manageable, others can pose significant risks and require prompt medical attention. Comprehensive care involving lifestyle changes, medications, and possibly interventional procedures can help control tachycardia and enhance quality of life for affected individuals.