Acute coronary syndrome (ACS) is a term used to describe a range of conditions associated with sudden, reduced blood flow to the heart. It encompasses conditions such as unstable angina, non-ST-elevation myocardial infarction (NSTEMI), and ST-elevation myocardial infarction (STEMI). Prompt diagnosis and treatment of ACS are crucial to prevent significant morbidity and mortality. This article provides a detailed overview of the diagnostic approach to ACS, including clinical assessment, electrocardiography (ECG), biomarkers, imaging, and risk stratification.
1. Clinical Assessment
The initial assessment of a patient suspected of having ACS is critical and involves a thorough history and physical examination.
SEE ALSO: What Are The Non-Modifiable Risk Factors for CAD?
History
Presenting Symptoms: The classic symptom of ACS is chest pain or discomfort. Patients often describe this pain as a pressure, tightness, or squeezing sensation. The pain is typically located in the central or left chest and may radiate to the left arm, neck, jaw, or back. It is important to note that some patients, particularly women, the elderly, and those with diabetes, may present with atypical symptoms such as shortness of breath, nausea, vomiting, epigastric pain, or syncope.
Duration and Onset: Acute chest pain that lasts more than a few minutes and is not relieved by rest or nitroglycerin should raise suspicion for ACS. Pain that occurs with exertion and is relieved by rest may indicate stable angina but warrants further evaluation.
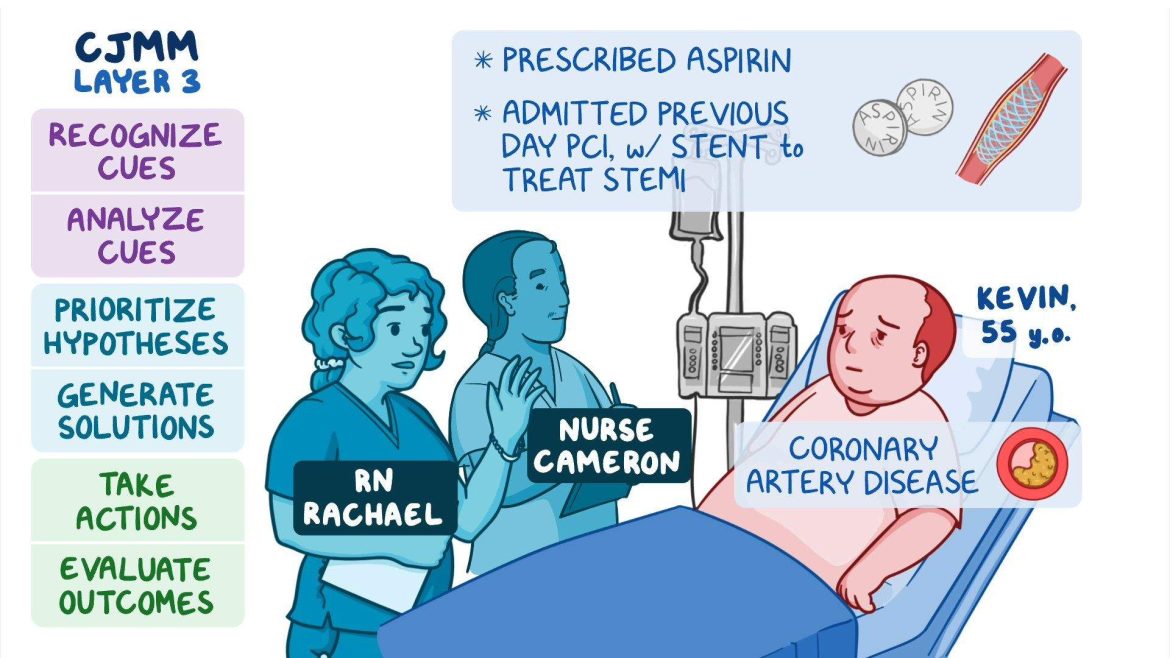
Risk Factors: Identifying risk factors for coronary artery disease (CAD) can aid in the diagnosis. Common risk factors include age, male gender, family history of CAD, hypertension, hyperlipidemia, smoking, diabetes, obesity, and a sedentary lifestyle.
Physical Examination
While the physical examination may be normal in patients with ACS, it can provide valuable clues. Key aspects to assess include:
Vital Signs: Hypotension, tachycardia, or bradycardia can indicate hemodynamic instability. Fever may suggest an underlying infectious process.
Cardiovascular Examination: Listen for abnormal heart sounds such as a new murmur (suggesting mitral regurgitation due to papillary muscle dysfunction), S3 or S4 gallops, or pericardial friction rub. Check for signs of heart failure, including jugular venous distention, rales, and peripheral edema.
Respiratory Examination: Evaluate for signs of pulmonary congestion or edema, which may indicate left ventricular dysfunction.
Abdominal Examination: Exclude other potential causes of chest pain, such as acute pancreatitis or peptic ulcer disease.
2. Electrocardiography (ECG)
ECG is a cornerstone in the diagnosis of ACS and should be performed within 10 minutes of patient presentation.
ST-Elevation Myocardial Infarction (STEMI)
ST-Segment Elevation: The hallmark of STEMI is ST-segment elevation in two or more contiguous leads. The criteria for significant ST-segment elevation vary with the anatomical location of the infarction:
Anterior STEMI: ST elevation in leads V1-V4.
Inferior STEMI: ST elevation in leads II, III, and aVF.
Lateral STEMI: ST elevation in leads I, aVL, V5, and V6.
Posterior STEMI: ST depression in leads V1-V3 with prominent R waves may indicate posterior involvement.
Non-ST-Elevation Myocardial Infarction (NSTEMI) and Unstable Angina
ST-Segment Depression and T-Wave Inversion: Patients with NSTEMI or unstable angina may present with ST-segment depression or T-wave inversion. These changes are less specific but suggest myocardial ischemia.
Serial ECGs
Dynamic Changes: Serial ECGs taken at 15-30 minute intervals can help detect dynamic changes in ST segments or T waves, which may not be evident on the initial ECG.
3. Cardiac Biomarkers
Cardiac biomarkers are essential in the diagnosis and risk stratification of ACS. The most commonly used biomarkers include troponins and creatine kinase-MB (CK-MB).
Troponins
Cardiac-Specific Troponins (cTnI and cTnT): Troponins are the preferred biomarkers due to their high sensitivity and specificity for myocardial injury. Elevated troponin levels confirm the diagnosis of myocardial infarction. Troponins rise within 3-6 hours after the onset of symptoms, peak at 12-24 hours, and remain elevated for up to 10-14 days.
Creatine Kinase-MB (CK-MB)
CK-MB: Although less specific than troponins, CK-MB can be useful in certain clinical scenarios. CK-MB levels rise within 3-6 hours, peak at 12-24 hours, and return to baseline within 48-72 hours.
Myoglobin
Myoglobin: Myoglobin is an early marker of myocardial injury, rising within 1-4 hours. However, its lack of specificity limits its utility in the diagnosis of ACS.
4. Imaging
Imaging modalities can provide additional information to support the diagnosis of ACS and assess for complications.
Echocardiography
Transthoracic Echocardiography (TTE): TTE can assess left ventricular function, wall motion abnormalities, and complications such as mitral regurgitation, ventricular septal defect, or pericardial effusion. It is particularly useful in patients with equivocal ECG findings or those with hemodynamic instability.
Coronary Angiography
Invasive Coronary Angiography: Coronary angiography remains the gold standard for identifying coronary artery occlusions. It is indicated in patients with STEMI and in high-risk NSTEMI patients or those with refractory symptoms despite medical therapy.
Cardiac Magnetic Resonance Imaging (MRI)
Cardiac MRI: Cardiac MRI provides detailed information on myocardial perfusion, viability, and the extent of myocardial damage. It is useful in cases where the diagnosis is uncertain or to assess for conditions such as myocarditis or takotsubo cardiomyopathy.
5. Risk Stratification
Risk stratification tools help identify patients at high risk for adverse outcomes and guide management decisions.
TIMI Risk Score
TIMI Risk Score for UA/NSTEMI: The TIMI (Thrombolysis in Myocardial Infarction) risk score is commonly used to stratify risk in patients with UA/NSTEMI. It incorporates seven variables:
Age ≥ 65 years
Three or more CAD risk factors
Known CAD (stenosis ≥ 50%)
Aspirin use in the past 7 days
Severe angina (≥ 2 episodes in 24 hours)
ST-segment deviation ≥ 0.5 mm
Elevated cardiac biomarkers
GRACE Risk Score
Global Registry of Acute Coronary Events (GRACE) Risk Score: The GRACE risk score is another widely used tool that predicts in-hospital and 6-month mortality in ACS patients. It includes variables such as age, heart rate, systolic blood pressure, creatinine level, cardiac arrest at presentation, ST-segment deviation, and elevated cardiac biomarkers.
Differential Diagnosis
It is essential to consider other potential causes of chest pain and exclude life-threatening conditions.
Differential Diagnoses to Consider
Aortic Dissection: Sudden, severe chest or back pain with a tearing quality. Hypertension and pulse deficits may be present.
Confirmed by CT angiography.
Pulmonary Embolism: Sudden onset of dyspnea, chest pain, and hypoxemia. D-dimer and CT pulmonary angiography can aid in diagnosis.
Pericarditis: Sharp, pleuritic chest pain that worsens with inspiration or lying flat. Pericardial friction rub may be present.
ECG shows diffuse ST elevation.
Pneumothorax: Sudden onset of unilateral chest pain and dyspnea.
Decreased breath sounds on the affected side. Confirmed by chest X-ray.
Gastroesophageal Reflux Disease (GERD): Burning chest pain associated with meals and relieved by antacids. Confirmed by history and response to treatment.
Conclusion
The diagnosis of acute coronary syndrome requires a multifaceted approach, integrating clinical assessment, ECG findings, cardiac biomarkers, and imaging studies. Prompt and accurate diagnosis is crucial for initiating appropriate therapy and improving patient outcomes. Clinicians must also consider alternative diagnoses and utilize risk stratification tools to guide management decisions. Continuous advancements in diagnostic modalities and biomarkers promise to enhance the early detection and treatment of ACS, ultimately reducing the burden of this life-threatening condition.