Heart failure is a serious and chronic condition in which the heart cannot pump enough blood to meet the body’s needs. As a result, essential organs like the brain, liver, and kidneys don’t receive enough oxygen and nutrients, leading to symptoms such as fatigue, shortness of breath, and swelling in the legs and ankles. There are various causes of heart failure, including coronary artery disease, high blood pressure, and cardiomyopathy. The condition can significantly impact the quality of life and is associated with a high mortality rate. This article explores whether a heart transplant can cure heart failure and examines the nuances and complexities involved.
Understanding Heart Failure
Heart failure is often classified into different types based on the part of the heart affected and the nature of the problem.
The most common classifications are:
Left-sided heart failure: This is the most common type and occurs when the left ventricle (the heart’s main pumping chamber) cannot pump blood efficiently. It can be further divided into systolic heart failure (reduced ejection fraction) and diastolic heart failure (preserved ejection fraction).
Right-sided heart failure: This occurs when the right ventricle has difficulty pumping blood to the lungs, leading to fluid buildup in the abdomen, legs, and feet.
Congestive heart failure: This term is often used interchangeably with heart failure and refers to the fluid buildup in various parts of the body due to the heart’s inability to pump effectively.
SEE ALSO: Is Heart Block The Same as Heart Failure?
Causes And Risk Factors
Several conditions and factors can lead to heart failure, including:
Coronary artery disease (CAD): Blocked or narrowed arteries reduce blood flow to the heart, leading to damage and weakening of the heart muscle.
High blood pressure (hypertension): Over time, elevated blood pressure can cause the heart to become too stiff or too weak to pump blood effectively.
Cardiomyopathy: This disease of the heart muscle can be caused by genetic factors, infections, alcohol abuse, or drug use.
Diabetes: This condition increases the risk of developing heart disease and heart failure.
Obesity: Excess body weight can contribute to heart failure by increasing the heart’s workload and the risk of developing other related conditions.
Treatment Options
Heart failure is a progressive condition that requires ongoing management. Treatment aims to improve symptoms, slow disease progression, and enhance the quality of life. Common treatments include:
Lifestyle changes: Dietary modifications, regular physical activity, weight management, and smoking cessation are critical components of heart failure management.
Medications: A variety of medications can help manage symptoms and improve heart function. These may include ACE inhibitors, beta-blockers, diuretics, aldosterone antagonists, and more.
Devices: Implantable devices such as pacemakers, defibrillators, and ventricular assist devices (VADs) can help manage heart rhythm problems and support heart function.
Surgery: In some cases, surgical interventions such as coronary artery bypass grafting (CABG), valve repair or replacement, or left ventricular assist device (LVAD) implantation may be necessary.
Heart Transplant as A Treatment Option
A heart transplant is considered when other treatments have failed to improve heart failure symptoms and quality of life.
This complex surgical procedure involves replacing the patient’s diseased heart with a healthy heart from a deceased donor.
It is typically reserved for patients with end-stage heart failure who have not responded to other treatments.
Indications for Heart Transplant
Candidates for heart transplantation typically meet several criteria, including:
Severe heart failure symptoms: Despite optimal medical therapy, the patient continues to experience significant symptoms and limitations in daily activities.
Poor prognosis: The patient has a poor prognosis without a transplant, with a high risk of death within a year.
No other treatment options: Other treatments, including medications and devices, have been exhausted and are no longer effective.
Absence of contraindications: The patient does not have conditions that would make the surgery excessively risky or preclude a successful outcome, such as active infections, cancer, or severe lung disease.
The Heart Transplant Process
The heart transplant process involves several steps:
Evaluation: Potential candidates undergo a comprehensive evaluation to determine their suitability for transplantation.
This includes assessing overall health, heart function, and the presence of any contraindications.
Waiting List: Once deemed suitable, the patient is placed on a national waiting list managed by the United Network for Organ Sharing (UNOS) in the United States or similar organizations in other countries. The waiting time can vary significantly based on factors such as blood type, body size, and the urgency of the patient’s condition.
Donor Matching: When a suitable donor heart becomes available, it is matched with the recipient based on factors such as blood type, size, and immunological compatibility. The patient is notified and must be ready to undergo the transplant surgery immediately.
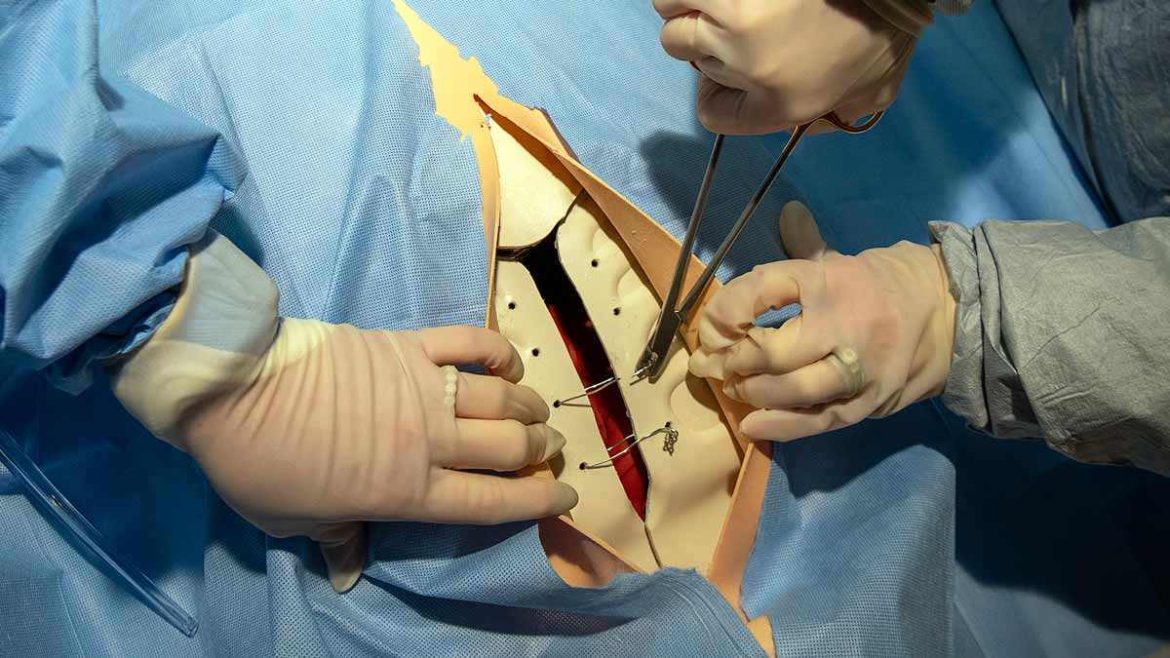
Surgery: The transplant surgery is performed under general anesthesia. The diseased heart is removed, and the donor heart is sewn into place. The surgery typically takes several hours.
Recovery and Rehabilitation: After the surgery, the patient is closely monitored in the intensive care unit (ICU) and gradually transitions to a regular hospital room. Rehabilitation involves physical therapy, medication management, and regular follow-up appointments to monitor heart function and overall health.
Outcomes And Prognosis
A heart transplant can offer a significant improvement in the quality of life and survival for patients with end-stage heart failure. According to data from the International Society for Heart and Lung Transplantation (ISHLT), the median survival rate after a heart transplant is approximately 12.5 years. Many patients experience dramatic improvements in their ability to perform daily activities and a substantial reduction in heart failure symptoms.
Survival Rates
Survival rates for heart transplant patients have improved over the years due to advances in surgical techniques, immunosuppressive medications, and post-transplant care. Some key statistics include:
One-year survival: Approximately 90% of heart transplant recipients survive the first year after surgery.
Five-year survival: Around 75% of recipients are alive five years post-transplant.
Ten-year survival: About 56% of recipients survive ten years or more after the transplant.
Complications And Challenges
While a heart transplant can be life-saving, it is not without risks and challenges. Some potential complications include:
Rejection
Rejection occurs when the body’s immune system recognizes the donor heart as foreign and attacks it. To prevent rejection, patients must take immunosuppressive medications for life. These medications help suppress the immune response but also increase the risk of infections and other side effects. Rejection can be acute (occurring within the first few months) or chronic (developing over years).
Infections
Immunosuppressive medications increase the risk of infections, as they weaken the immune system. Patients are closely monitored for signs of infection and may require prophylactic antibiotics or antiviral medications to prevent serious infections.
Graft Vasculopathy
Cardiac allograft vasculopathy (CAV) is a condition in which the blood vessels of the transplanted heart become narrowed or blocked, leading to reduced blood flow and potential heart failure. CAV is a leading cause of long-term transplant failure and requires ongoing monitoring and management.
Medication Side Effects
Immunosuppressive medications can have various side effects, including kidney damage, high blood pressure, diabetes, and an increased risk of certain cancers. Balancing the benefits and risks of these medications is a critical aspect of post-transplant care.
Conclusion
Can a heart transplant cure heart failure? The answer depends on how we define “cure.” A heart transplant can dramatically improve the quality of life and survival for patients with end-stage heart failure, effectively alleviating symptoms and restoring the ability to perform daily activities. For many, it offers a new lease on life and the potential for many more years of active living.