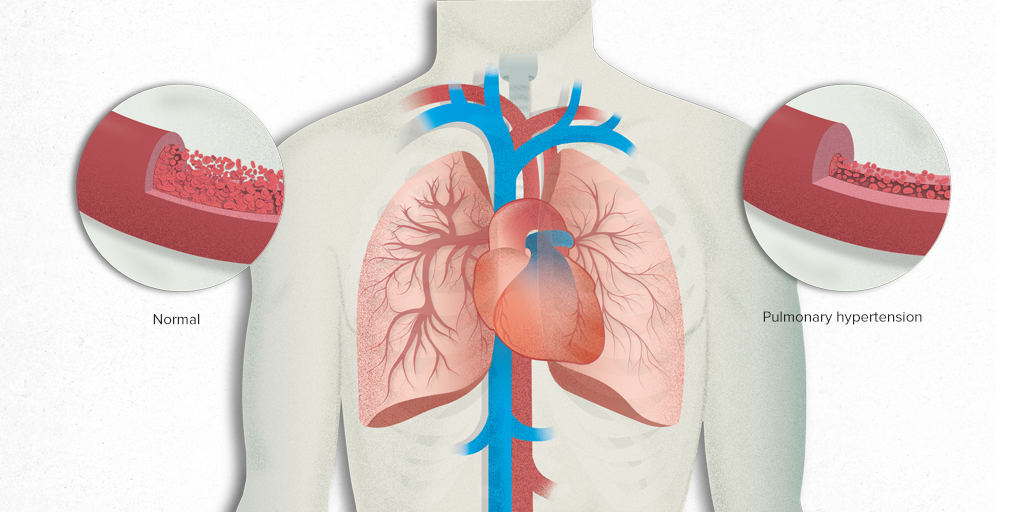
Pulmonary hypertension (PH) is a condition characterized by elevated blood pressure in the pulmonary arteries, the vessels that carry blood from the heart to the lungs. This elevated pressure can lead to a range of complications, significantly affecting the quality of life and overall prognosis of those afflicted. However, whether pulmonary hypertension should be classified as a respiratory disease remains a topic of discussion and investigation among medical professionals. This article aims to explore the nature of pulmonary hypertension, its causes, effects, and its classification in the context of respiratory diseases.
What Is Pulmonary Hypertension?
Pulmonary hypertension is not a single disease but rather a complex condition with various underlying causes and manifestations. It is defined by an increase in mean pulmonary arterial pressure (mPAP) to 25 mmHg or more at rest, as determined by right heart catheterization. This elevation in pressure can result from a variety of pathological mechanisms affecting the pulmonary vasculature.
SEE ALSO: What Bread Lowers Blood Pressure?
Classifications of Pulmonary Hypertension
The World Health Organization (WHO) has classified pulmonary hypertension into five distinct groups based on their underlying causes:
Pulmonary Arterial Hypertension (PAH): This group includes idiopathic, heritable, and drug- or toxin-induced forms of PAH, as well as those associated with connective tissue diseases, congenital heart diseases, and certain infections.
Pulmonary Hypertension due to Left Heart Disease: This group encompasses conditions such as left ventricular systolic or diastolic dysfunction, as well as valvular diseases that lead to elevated pressure in the pulmonary arteries.
Pulmonary Hypertension due to Lung Diseases and/or Hypoxia: This group includes chronic obstructive pulmonary disease (COPD), interstitial lung diseases, and other conditions that cause chronic hypoxia and subsequently lead to pulmonary hypertension.
Chronic Thromboembolic Pulmonary Hypertension (CTEPH): This group is characterized by persistent pulmonary hypertension due to unresolved blood clots in the pulmonary arteries.
Pulmonary Hypertension with Unclear Multifactorial Mechanisms: This group includes conditions that do not fit neatly into the other categories and may involve multiple contributing factors.
Pathophysiology of Pulmonary Hypertension
The pathophysiology of pulmonary hypertension is complex and involves various mechanisms. The primary changes include vasoconstriction, vascular remodeling, thrombosis in situ, and inflammation. These changes lead to increased pulmonary vascular resistance, which in turn causes elevated pulmonary arterial pressure.
Vasoconstriction: The narrowing of pulmonary arteries due to smooth muscle contraction.
Vascular Remodeling: Structural changes in the pulmonary arteries, including smooth muscle cell proliferation and fibrosis.
Thrombosis in Situ: The formation of blood clots within the pulmonary arteries.
Inflammation: Inflammatory processes that contribute to vascular damage and remodeling.
Pulmonary Hypertension And Respiratory Diseases
To understand whether pulmonary hypertension is a respiratory disease, it is crucial to examine its relationship with various respiratory conditions.
Pulmonary Hypertension due to Lung Diseases and/or Hypoxia
This category of pulmonary hypertension is directly related to respiratory diseases. Conditions such as COPD, interstitial lung diseases, and obstructive sleep apnea can lead to chronic hypoxia, which subsequently causes pulmonary hypertension. In these cases, pulmonary hypertension is a secondary condition resulting from primary respiratory diseases.
Chronic Obstructive Pulmonary Disease (COPD): COPD is a common cause of pulmonary hypertension. The chronic inflammation and destruction of lung tissue in COPD lead to hypoxia and subsequent pulmonary vascular changes, resulting in elevated pulmonary arterial pressure.
Interstitial Lung Diseases (ILD): ILDs, such as idiopathic pulmonary fibrosis, cause scarring and stiffening of lung tissue.
This impairs oxygen exchange, leading to hypoxia and pulmonary hypertension.
Obstructive Sleep Apnea (OSA): OSA is characterized by repeated episodes of upper airway obstruction during sleep, leading to intermittent hypoxia. This can result in pulmonary vasoconstriction and eventually pulmonary hypertension.
Pulmonary Arterial Hypertension (PAH)
Pulmonary arterial hypertension (PAH) is a primary form of pulmonary hypertension that can occur independently of other diseases. While it primarily affects the pulmonary arteries, it is not typically classified as a respiratory disease. Instead, PAH is considered a vascular disorder.
However, it is important to note that PAH can lead to secondary respiratory complications due to its impact on the pulmonary circulation.
Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
CTEPH is another form of pulmonary hypertension that is not primarily a respiratory disease. It results from chronic blood clots in the pulmonary arteries, which obstruct blood flow and increase pressure. While CTEPH affects the pulmonary vasculature, it is more accurately classified as a vascular and thromboembolic disorder.
Diagnostic Approaches
The diagnosis of pulmonary hypertension involves a combination of clinical evaluation, imaging studies, and hemodynamic measurements.
1. Clinical Evaluation
A thorough clinical history and physical examination are essential for diagnosing pulmonary hypertension. Symptoms such as dyspnea (shortness of breath), fatigue, chest pain, and syncope (fainting) are common but nonspecific. Physical findings may include signs of right ventricular hypertrophy and heart failure.
2. Imaging Studies
Echocardiography: This non-invasive imaging technique is often the first step in evaluating suspected pulmonary hypertension. It can estimate pulmonary arterial pressure and assess right ventricular function.
Chest X-ray and Computed Tomography (CT): These imaging modalities can provide information about lung parenchyma, pulmonary arteries, and other potential causes of pulmonary hypertension.
Ventilation-Perfusion (V/Q) Scan: This nuclear medicine test is useful for detecting chronic thromboembolic pulmonary hypertension.
3. Hemodynamic Measurements
Right Heart Catheterization: This invasive procedure is the gold standard for diagnosing pulmonary hypertension. It provides direct measurements of pulmonary arterial pressure, pulmonary capillary wedge pressure, and cardiac output.
Treatment Approaches
The management of pulmonary hypertension depends on its underlying cause and severity. Treatment strategies aim to alleviate symptoms, improve quality of life, and slow disease progression.
General Measures
Oxygen Therapy: Supplemental oxygen can help alleviate hypoxia in patients with respiratory diseases and hypoxic pulmonary hypertension.
Diuretics: These medications help manage fluid retention and reduce symptoms of right heart failure.
Anticoagulation: In cases of CTEPH, anticoagulant therapy is essential to prevent further thromboembolic events.
Targeted Therapies
For patients with PAH, targeted therapies aim to address the underlying vascular pathology:
Endothelin Receptor Antagonists (ERAs): These drugs block the effects of endothelin-1, a potent vasoconstrictor, thereby reducing pulmonary vascular resistance.
Phosphodiesterase-5 Inhibitors (PDE-5 inhibitors): These medications promote vasodilation by increasing the availability of cyclic guanosine monophosphate (cGMP).
Prostacyclin Analogues: These drugs mimic the effects of prostacyclin, a vasodilator and inhibitor of platelet aggregation.
Soluble Guanylate Cyclase (sGC) Stimulators: These medications enhance the nitric oxide signaling pathway, leading to vasodilation.
Surgical Interventions
Pulmonary Endarterectomy (PEA): This surgical procedure is the treatment of choice for CTEPH. It involves the removal of organized thromboembolic material from the pulmonary arteries.
Lung Transplantation: In advanced cases of pulmonary hypertension, lung transplantation may be considered when other treatments have failed.
Conclusion
Pulmonary hypertension is a complex condition that intersects with both respiratory and vascular domains. While certain forms of pulmonary hypertension, such as those due to lung diseases and hypoxia, can be closely linked to respiratory conditions, others, like PAH and CTEPH, are primarily vascular disorders with secondary respiratory implications.
Therefore, pulmonary hypertension cannot be universally classified as a respiratory disease. Instead, its classification depends on the underlying cause and pathophysiological mechanisms.