Heart failure is a severe condition affecting millions worldwide, characterized by the heart’s inability to pump blood efficiently. Among those afflicted, understanding the most common cause of death is crucial for both prevention and treatment strategies.
Introduction
Heart failure, a progressive and debilitating condition, impacts approximately 26 million people globally. It is a significant public health issue that leads to frequent hospitalizations, reduced quality of life, and a high mortality rate. Despite advances in medical treatment, the prognosis for heart failure patients remains poor. Understanding the most common cause of death among these patients can help healthcare providers develop better treatment plans and preventive measures to improve patient outcomes.
SEE ALSO: How Long Can You Live with Low Heart Function
The Mechanism of Heart Failure
Heart failure occurs when the heart muscle becomes weakened or stiff, impairing its ability to pump blood effectively. This can result from various conditions, including coronary artery disease, high blood pressure, and diabetes. The reduced pumping efficiency causes blood to back up in the veins, leading to fluid accumulation in the lungs, liver, and other parts of the body. Symptoms of heart failure include shortness of breath, fatigue, swollen legs, and rapid heartbeat.
The Importance of Identifying Common Causes of Death
Identifying the most common causes of death in heart failure patients is vital for several reasons. Firstly, it allows healthcare providers to focus on high-risk areas, improving patient monitoring and intervention strategies. Secondly, it informs the development of guidelines and protocols aimed at reducing mortality rates. Lastly, it helps patients and their families understand the risks and engage more actively in managing the condition.
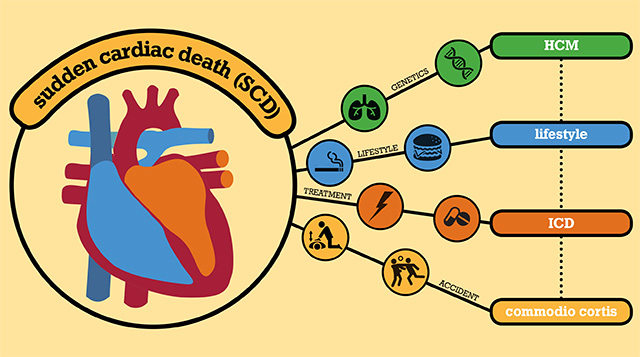
Sudden Cardiac Death: The Leading Cause
The most common cause of death in people with heart failure is sudden cardiac death (SCD). Sudden cardiac death accounts for approximately 30-50% of all deaths in heart failure patients. SCD is defined as an unexpected death due to cardiac causes within one hour of symptom onset. It is often caused by ventricular arrhythmias, which are abnormal heart rhythms originating from the lower chambers of the heart.
Understanding Ventricular Arrhythmias
Ventricular arrhythmias include ventricular tachycardia (VT) and ventricular fibrillation (VF). VT is a rapid heart rate that starts in the ventricles, while VF is a chaotic, irregular heart rhythm that can lead to cardiac arrest. Both conditions disrupt the heart’s ability to pump blood effectively, leading to a sudden and severe drop in blood pressure and loss of consciousness.
Risk Factors for Sudden Cardiac Death
Several factors increase the risk of SCD in heart failure patients:
Reduced Ejection Fraction: A lower ejection fraction (EF) indicates a more severe impairment in the heart’s pumping ability. Patients with an EF below 35% are at higher risk for SCD.
Previous Myocardial Infarction: A history of heart attacks can lead to scar tissue in the heart, which can disrupt electrical signals and increase the likelihood of arrhythmias.
Heart Failure Class: Patients in higher New York Heart Association (NYHA) functional classes (III and IV) are at greater risk due to more advanced heart failure.
Electrolyte Imbalances: Imbalances in potassium, magnesium, and calcium levels can trigger arrhythmias.
Genetic Factors: Certain genetic mutations can predispose individuals to arrhythmias and SCD.
Other Causes of Death in Heart Failure Patients
While SCD is the leading cause, other factors also contribute significantly to mortality in heart failure patients. These include:
Progressive Heart Failure
Progressive heart failure is the second most common cause of death, accounting for about 30-40% of heart failure-related deaths. This occurs when the heart’s function continues to decline despite treatment, leading to worsening symptoms and organ failure. Patients may experience severe fluid retention, difficulty breathing, and extreme fatigue in the advanced stages.
Non-Cardiovascular Causes
Non-cardiovascular causes, such as infections, renal failure, and malignancies, contribute to the remaining 20-30% of deaths. Heart failure patients are often more susceptible to infections due to weakened immune systems and frequent hospitalizations. Additionally, the chronic stress of managing heart failure can lead to other health complications, further increasing mortality risk.
Strategies to Reduce Mortality in Heart Failure Patients
Given the high mortality rate associated with heart failure, it is crucial to implement strategies to reduce the risk of death.
These strategies include:
Medication Management
Medications play a vital role in managing heart failure and reducing mortality. Key medications include:
ACE Inhibitors and ARBs: These drugs help relax blood vessels, reduce blood pressure, and decrease the workload on the heart.
Beta-Blockers: Beta-blockers slow the heart rate and reduce blood pressure, helping to improve heart function.
Aldosterone Antagonists: These medications help remove excess fluid and reduce the risk of hospitalization and death.
SGLT2 Inhibitors: Originally used for diabetes management, these drugs have been shown to reduce heart failure-related deaths.
Device Therapy
Implantable devices can significantly reduce the risk of SCD in heart failure patients:
Implantable Cardioverter-Defibrillators (ICDs): ICDs monitor heart rhythms and deliver shocks to restore normal rhythms if a dangerous arrhythmia is detected.
Cardiac Resynchronization Therapy (CRT): CRT devices help improve the coordination of the heart’s contractions, enhancing its efficiency and reducing symptoms.
Lifestyle Modifications
Lifestyle changes can also play a crucial role in managing heart failure and reducing mortality risk:
Diet and Nutrition: A heart-healthy diet low in sodium and saturated fats can help manage blood pressure and reduce fluid retention.
Exercise: Regular physical activity can improve heart function and overall cardiovascular health.
Smoking Cessation: Quitting smoking can significantly reduce the risk of heart disease and improve outcomes for heart failure patients.
Alcohol Moderation: Limiting alcohol intake can help prevent further damage to the heart.
Regular Monitoring and Follow-Up
Frequent monitoring and follow-up with healthcare providers are essential for managing heart failure effectively. This includes:
Regular Check-Ups: Routine visits to the cardiologist to monitor heart function and adjust treatment plans as needed.
Self-Monitoring: Patients should monitor their weight, blood pressure, and symptoms daily to detect any changes early.
Education and Support: Providing patients and their families with education about heart failure and support resources can improve adherence to treatment plans and quality of life.
Conclusion
Heart failure is a complex and life-threatening condition with high mortality rates. Sudden cardiac death, primarily caused by ventricular arrhythmias, is the most common cause of death in heart failure patients. Understanding this and other contributing factors is crucial for developing effective treatment and prevention strategies. By managing risk factors, adhering to medication regimens, utilizing device therapy, and making lifestyle modifications, patients can improve their outcomes and quality of life.