Hyperlipidemia, characterized by elevated levels of lipids in the blood, is a major risk factor for cardiovascular diseases (CVDs) including coronary artery disease, stroke, and peripheral artery disease. Effective management of hyperlipidemia is crucial in reducing the risk of these potentially life-threatening conditions. The first-line management of hyperlipidemia involves a combination of lifestyle modifications and pharmacotherapy aimed at lowering lipid levels and improving overall cardiovascular health.
Risk Assessment
Before initiating treatment, it is essential to assess the patient’s overall cardiovascular risk. This involves evaluating factors such as age, gender, family history, smoking status, hypertension, diabetes, and existing CVD. Various risk assessment tools, such as the Framingham Risk Score and the ASCVD Risk Estimator, can help determine the patient’s risk level and guide treatment decisions.
What Is The First-line Management of Hyperlipidemia?
Dietary modification, weight loss, and exercise are the first line of defense. Patients at higher risk for cardiovascular events (cardiovascular death, nonfatal myocardial infarction, nonfatal stroke, coronary revascularization, or unstable angina) may benefit from lipid-lowering drugs.
SEE ALSO: How Long Does It Take to Lower Cholesterol with Exercise
Lifestyle Modifications
1. Diet
A heart-healthy diet is fundamental in the management of hyperlipidemia. Key dietary recommendations include:
Reducing Saturated and Trans Fats: Saturated fats, found in red meat, butter, and full-fat dairy products, should be limited as they raise LDL-C levels. Trans fats, found in processed and fried foods, should be avoided as they not only increase LDL-C but also lower HDL-C.
Increasing Fiber Intake: Soluble fiber, found in oats, fruits, vegetables, and legumes, helps lower LDL-C by binding to cholesterol in the digestive system and preventing its absorption.
Incorporating Healthy Fats: Monounsaturated and polyunsaturated fats, found in olive oil, nuts, seeds, and fatty fish, can help improve lipid profiles.
Plant Sterols and Stanols: These compounds, found in fortified foods and supplements, can help reduce LDL-C levels by blocking cholesterol absorption in the intestine.
Reducing Dietary Cholesterol: While dietary cholesterol has a smaller effect on blood cholesterol levels compared to saturated and trans fats, it is still advisable to limit intake from sources such as egg yolks and shellfish.
2. Physical Activity
Regular physical activity can help improve lipid levels, reduce blood pressure, and promote weight loss. The American Heart
Association (AHA) recommends at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week, along with muscle-strengthening activities on two or more days per week.
3. Weight Management
Achieving and maintaining a healthy weight is crucial for managing hyperlipidemia. Weight loss can significantly lower LDL-C, triglycerides, and total cholesterol while increasing HDL-C. A combination of dietary changes and increased physical activity is the most effective approach to weight management.
4. Smoking Cessation
Smoking cessation is vital for reducing cardiovascular risk. Smoking negatively affects lipid profiles by lowering HDL-C and raising LDL-C and triglycerides. Additionally, smoking contributes to endothelial dysfunction, inflammation, and thrombosis, further increasing CVD risk.
5. Limiting Alcohol Intake
Excessive alcohol consumption can raise triglyceride levels and contribute to weight gain. It is recommended to limit alcohol intake to moderate levels, defined as up to one drink per day for women and up to two drinks per day for men.
Pharmacotherapy
When lifestyle modifications alone are insufficient to achieve lipid goals, pharmacotherapy is indicated. The choice of medication depends on the patient’s specific lipid abnormalities, overall cardiovascular risk, and any underlying health conditions.
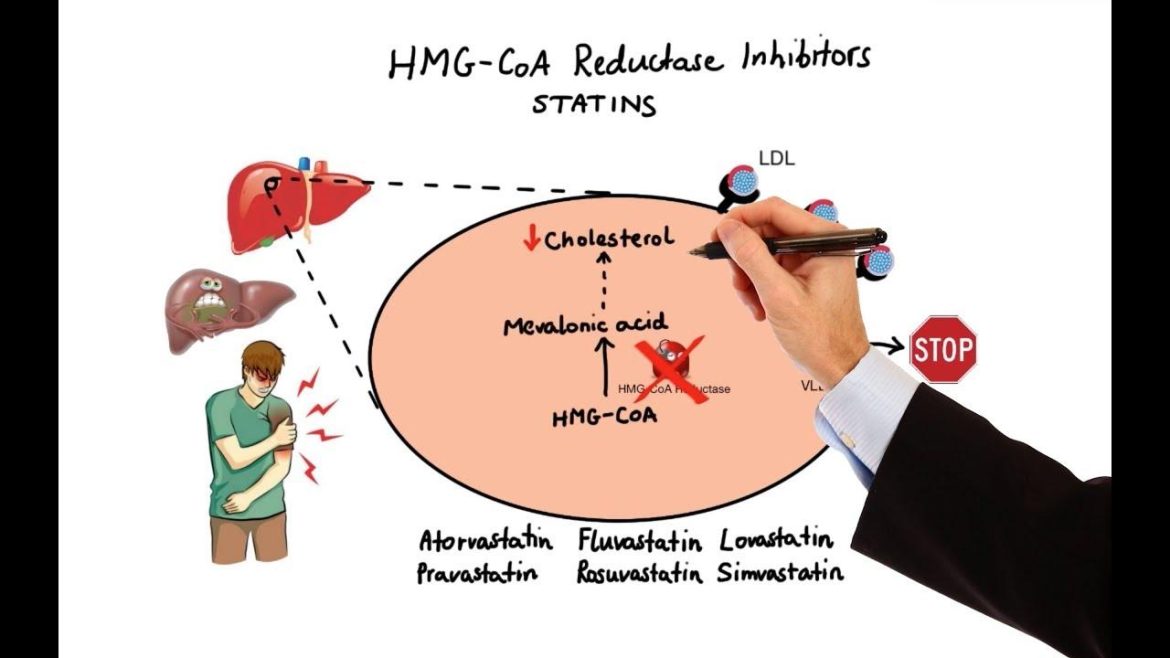
Statins
1. Mechanism of Action
Statins are the cornerstone of pharmacotherapy for hyperlipidemia. They work by inhibiting HMG-CoA reductase, an enzyme involved in cholesterol synthesis in the liver. This leads to an upregulation of LDL receptors on hepatocytes, increasing the clearance of LDL-C from the blood.
2. Efficacy
Statins effectively lower LDL-C levels by 20-60%, depending on the specific statin and dose. They also modestly reduce triglycerides and increase HDL-C levels. Importantly, statins have been shown to reduce the incidence of major cardiovascular events, including myocardial infarction and stroke.
3. Side Effects
Common side effects of statins include muscle pain, liver enzyme elevations, and, rarely, myopathy and rhabdomyolysis.
Regular monitoring of liver enzymes and creatine kinase levels is recommended to detect and manage potential side effects.
Ezetimibe
1. Mechanism of Action
Ezetimibe works by inhibiting the absorption of cholesterol in the small intestine, leading to a reduction in the amount of cholesterol delivered to the liver and an increase in LDL receptor activity.
2. Efficacy
Ezetimibe can lower LDL-C levels by 15-20% and is often used as an add-on therapy to statins when additional LDL-C reduction is needed.
3. Side Effects
Ezetimibe is generally well-tolerated, with the most common side effects being gastrointestinal disturbances and elevated liver enzymes when combined with statins.
PCSK9 Inhibitors
1. Mechanism of Action
PCSK9 inhibitors are monoclonal antibodies that inhibit the protein PCSK9, which degrades LDL receptors on hepatocytes. By blocking PCSK9, these medications increase the number of LDL receptors available to clear LDL-C from the blood.
2. Efficacy
PCSK9 inhibitors, such as alirocumab and evolocumab, can lower LDL-C levels by 50-60% and are particularly useful in patients with familial hypercholesterolemia or those who do not achieve lipid goals with statins and ezetimibe.
3. Side Effects
Common side effects include injection site reactions, upper respiratory tract infections, and flu-like symptoms. PCSK9 inhibitors are administered via subcutaneous injection every two to four weeks.
Bile Acid Sequestrants
1. Mechanism of Action
Bile acid sequestrants, such as cholestyramine, colestipol, and colesevelam, bind to bile acids in the intestine, preventing their reabsorption. This forces the liver to use more cholesterol to produce bile acids, thereby lowering LDL-C levels.
2. Efficacy
Bile acid sequestrants can lower LDL-C levels by 15-30%. They are often used in combination with statins for additional LDL-C reduction.
3. Side Effects
Common side effects include gastrointestinal disturbances, such as constipation, bloating, and nausea. They can also interfere with the absorption of other medications and fat-soluble vitamins.
Niacin
1. Mechanism of Action
Niacin, also known as vitamin B3, inhibits the synthesis of VLDL and LDL in the liver and increases HDL-C levels by reducing the clearance of HDL.
2. Efficacy
Niacin can lower LDL-C and triglycerides by 10-20% and increase HDL-C by 15-35%. However, its use has declined due to side effects and the availability of more effective therapies.
3. Side Effects
Common side effects include flushing, gastrointestinal disturbances, and elevated liver enzymes. Niacin can also increase blood glucose levels, making it less suitable for patients with diabetes.
Monitoring and Follow-Up
Regular monitoring and follow-up are essential components of hyperlipidemia management. Lipid levels should be reassessed 4-12 weeks after initiating or changing therapy and every 3-12 months thereafter to ensure treatment goals are met. Additionally, monitoring for potential side effects and adherence to lifestyle modifications and medication is crucial for long-term success.
Patient Education And Support
Educating patients about the importance of lipid management, lifestyle modifications, and medication adherence is vital. Support from healthcare providers, dietitians, and pharmacists can enhance patient understanding and motivation.
Behavioral counseling and community resources, such as smoking cessation programs and weight management groups, can also provide valuable support.
Conclusion
The first-line management of hyperlipidemia involves a comprehensive approach combining lifestyle modifications and pharmacotherapy tailored to the individual’s risk profile and lipid abnormalities. Lifestyle changes, including a heart-healthy diet, regular physical activity, weight management, smoking cessation, and limiting alcohol intake, form the foundation of treatment. Pharmacotherapy, primarily with statins, ezetimibe, and PCSK9 inhibitors, is employed when lifestyle interventions are insufficient to achieve lipid goals.