The vagus nerve, also known as the tenth cranial nerve or cranial nerve X, plays a critical role in the autonomic nervous system, regulating various bodily functions including heart rate, digestion, and respiratory rate. Premature VentricularContractions (PVCs) are extra heartbeats originating from the ventricles, which disrupt the regular heart rhythm.
This article delves into the potential connection between the vagus nerve and PVCs, exploring the mechanisms, symptoms, diagnostic approaches, and potential treatments.
What Is The Vagus Nerve?
The vagus nerve is the longest cranial nerve, extending from the brainstem to the abdomen, and influences the heart, lungs, and digestive tract. It has both sensory and motor functions and is a key component of the parasympathetic nervous system. The vagus nerve helps to slow the heart rate, promote digestion, and manage various involuntary processes essential for homeostasis.
SEE ALSO: How Do I Know If my Heartbeat Is Irregular?
Functions of The Vagus Nerve
Cardiac Regulation: The vagus nerve helps modulate heart rate by reducing the firing rate of the sinoatrial (SA) node, thus slowing down the heart rate.
Digestive Processes: It stimulates peristalsis and the production of digestive enzymes, promoting efficient digestion.
Respiratory Control: It influences breathing by modulating the respiratory rate.
Inflammation Control: The vagus nerve has anti-inflammatory effects through the cholinergic anti-inflammatory pathway.
Premature Ventricular Contractions (PVCs): An Overview
PVCs are a type of arrhythmia where the ventricles contract earlier than expected in the cardiac cycle. These extra beats are usually harmless but can be symptomatic and distressing for some individuals.
Characteristics of PVCs
Ectopic Beats: PVCs originate from ectopic foci in the ventricles rather than from the SA node.
Irregular Heartbeat: They can create a sensation of skipped or extra beats.
Symptoms: Patients may experience palpitations, dizziness, or chest discomfort, although many are asymptomatic.
Potential Mechanisms Linking The Vagus Nerve And PVCs
The connection between the vagus nerve and PVCs can be understood through several potential mechanisms:
Vagal Stimulation and Heart Rate: Increased vagal tone can slow the heart rate, creating a longer diastolic period which may predispose to ectopic activity in the ventricles.
Autonomic Imbalance: Imbalance between sympathetic and parasympathetic activity, with excessive vagal tone, can trigger PVCs.
Reflex Pathways: The vagus nerve can influence reflex pathways that may lead to ventricular ectopic activity.
Vagal Maneuvers And PVCs
Vagal maneuvers, such as the Valsalva maneuver or carotid sinus massage, are techniques that stimulate the vagus nerve.
These maneuvers are often used to terminate supraventricular tachycardia but can also affect the occurrence of PVCs.
Clinical Evidence And Research
Several studies have explored the relationship between vagal activity and PVCs:
Electrophysiological Studies: These studies have shown that increased vagal tone can lead to a higher incidence of PVCs, especially in patients with existing heart conditions.
Case Reports: Some case reports suggest that vagal maneuvers can induce or exacerbate PVCs in certain individuals.
Holter Monitoring: Continuous monitoring has revealed that periods of increased vagal tone, such as during sleep or rest, are associated with higher PVC frequency.
Pathophysiological Insights
The underlying pathophysiology may involve:
Ventricular Repolarization: Vagal stimulation affects ventricular repolarization, potentially leading to ectopic beats.
Ion Channel Modulation: Vagal activity influences ion channels in the cardiac cells, affecting the electrical stability of the ventricles.
Diagnosis And Evaluation
Diagnosing the role of the vagus nerve in PVCs involves a comprehensive evaluation:
Electrocardiogram (ECG): Identifies PVCs and helps assess their frequency and pattern.
Holter Monitoring: Provides continuous ECG recording to correlate PVCs with daily activities and autonomic tone.
Autonomic Testing: Assesses vagal function through heart rate variability (HRV) and other autonomic tests.
Stress Tests: Evaluates the effect of exercise and autonomic changes on PVC frequency.
Differential Diagnosis
It is crucial to differentiate PVCs induced by vagal activity from other causes such as:
Electrolyte Imbalances: Potassium, magnesium, and calcium levels should be evaluated.
Structural Heart Disease: Echocardiography and other imaging modalities can rule out underlying structural abnormalities.
Medications: Certain medications can influence vagal tone and should be reviewed.
Management And Treatment
Management strategies focus on addressing the underlying vagal influence and reducing PVC frequency:
Lifestyle Modifications: Reducing stress, avoiding excessive alcohol and caffeine, and ensuring adequate sleep can help modulate vagal tone.
Medications: Beta-blockers and calcium channel blockers can help reduce PVC frequency by modulating autonomic tone.
Ablation Therapy: In refractory cases, catheter ablation may be considered to target specific ectopic foci.
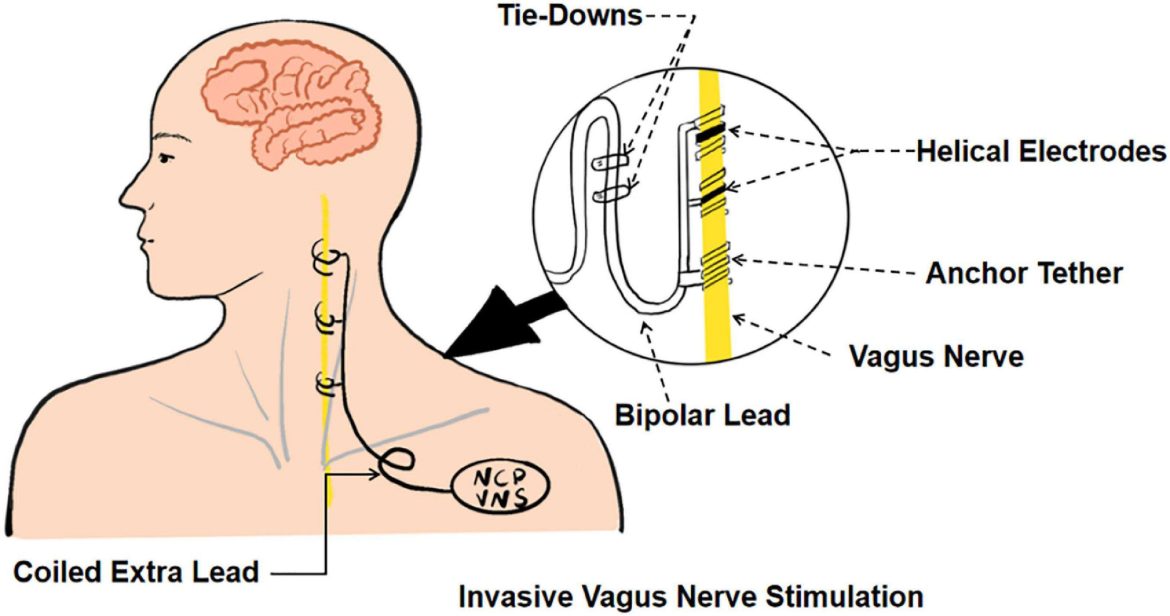
Vagal Modulation: Techniques such as biofeedback and vagal nerve stimulation (VNS) can be explored for their potential benefits in reducing PVCs.
Vagal Nerve Stimulation (VNS)
VNS involves electrical stimulation of the vagus nerve and is primarily used for epilepsy and depression. Its role in managing PVCs is still under investigation but shows promise in modulating autonomic tone.
Conclusion
The vagus nerve can influence the occurrence of PVCs through various mechanisms involving autonomic regulation and ventricular electrophysiology. While increased vagal tone can predispose individuals to PVCs, the relationship is complex and multifactorial. Understanding this connection can help in the effective diagnosis and management of PVCs, particularly in individuals with heightened vagal activity. Further research is needed to elucidate the precise pathways and develop targeted treatments for vagally-mediated PVCs.