The left ventricle, the largest and most muscular chamber of the heart, plays a pivotal role in pumping oxygen-rich blood to the rest of the body. Its efficient function is crucial for overall cardiovascular health. However, several conditions and factors can lead to left ventricle problems, compromising its ability to function properly and potentially leading to serious health issues. This article delves into the primary causes of left ventricle problems, providing a comprehensive understanding of their origins, implications, and the importance of early detection and management.
What Causes Left Ventricle Problems
1. Coronary Artery Disease (CAD)
Atherosclerosis and Its Impact
Coronary artery disease, primarily caused by atherosclerosis, is a leading cause of left ventricle problems. Atherosclerosis involves the buildup of plaque (composed of fat, cholesterol, and other substances) in the coronary arteries, which supply blood to the heart muscle. This buildup narrows the arteries, reducing blood flow to the left ventricle and other parts of the heart. Over time, reduced blood flow can weaken the left ventricle, leading to ischemic cardiomyopathy, a condition where the heart muscle is damaged due to insufficient blood supply.
see also: How Long Can You Live with LV Dysfunction
Myocardial Infarction
A myocardial infarction (heart attack) occurs when a coronary artery is completely blocked, cutting off blood supply to a part of the heart muscle. If the affected area includes the left ventricle, the muscle tissue can become damaged or die, resulting in weakened heart function and potential heart failure. Repeated heart attacks can exacerbate this damage, further compromising left ventricle function.
2. Hypertension (High Blood Pressure)
Increased Workload and Hypertrophy
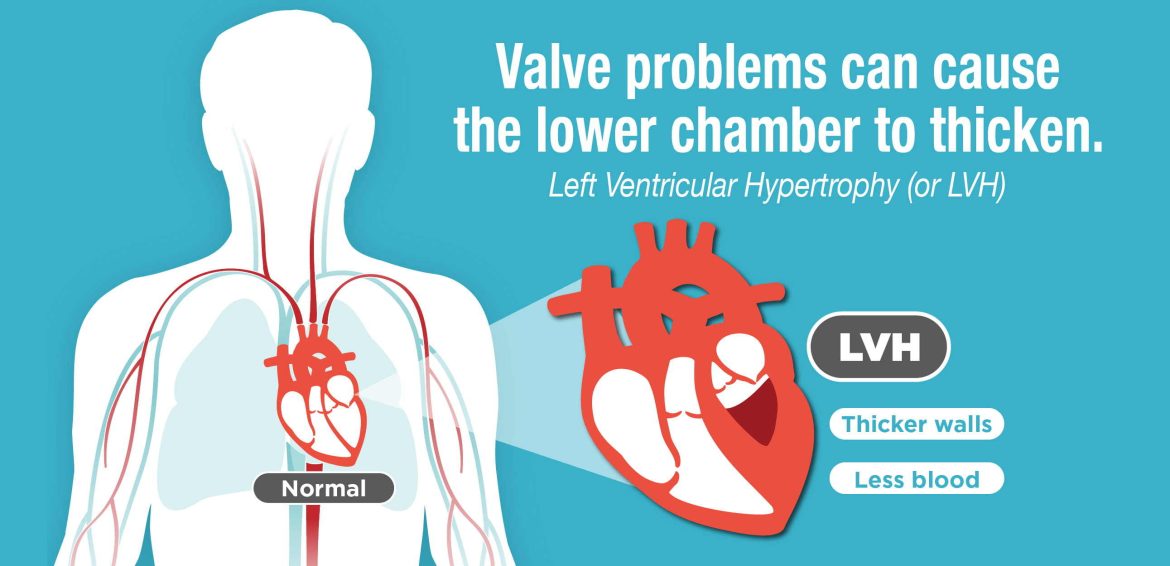
Chronic high blood pressure forces the left ventricle to work harder to pump blood against increased resistance in the arteries. Over time, this increased workload causes the left ventricle to thicken and enlarge, a condition known as left ventricular hypertrophy (LVH). While initially a compensatory mechanism, LVH can lead to stiffening of the heart muscle, impaired relaxation, and eventually heart failure. Persistent hypertension is a significant risk factor for developing left ventricle problems.
3. Cardiomyopathy
Dilated Cardiomyopathy
Dilated cardiomyopathy (DCM) is characterized by the enlargement and weakening of the left ventricle. This condition impairs the heart’s ability to pump blood efficiently, leading to reduced cardiac output and potential heart failure. The exact cause of DCM is often unknown, but it can be linked to genetic factors, infections, toxins, and other medical conditions.
Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy (HCM) involves abnormal thickening of the heart muscle, particularly the left ventricle.
Unlike LVH caused by hypertension, HCM is often hereditary. The thickened muscle can obstruct blood flow out of the heart, leading to symptoms such as chest pain, shortness of breath, and arrhythmias. In severe cases, HCM can cause sudden cardiac death.
Restrictive Cardiomyopathy
Restrictive cardiomyopathy is characterized by the stiffening of the heart muscle, which restricts the left ventricle’s ability to fill properly during diastole (the relaxation phase of the cardiac cycle). This condition can result from various underlying causes, including amyloidosis, sarcoidosis, and fibrosis. The reduced filling capacity leads to decreased cardiac output and symptoms of heart failure.
4. Valve Disorders
Aortic Stenosis
Aortic stenosis occurs when the aortic valve, which allows blood to flow from the left ventricle to the aorta, becomes narrowed or obstructed. This condition forces the left ventricle to work harder to push blood through the narrowed valve, leading to hypertrophy and eventual left ventricle dysfunction. Over time, the increased workload can result in heart failure if not treated promptly.
Mitral Regurgitation
Mitral regurgitation involves the backflow of blood from the left ventricle into the left atrium due to a malfunctioning mitral valve. This backflow increases the volume load on the left ventricle, causing it to dilate and eventually weaken.
Chronic mitral regurgitation can lead to heart failure and other complications if not addressed.
5. Myocarditis
Inflammation of the Heart Muscle: Myocarditis is the inflammation of the heart muscle, often caused by viral infections, but it can also result from bacterial infections, autoimmune diseases, or exposure to toxins. Inflammation can damage the left ventricle, impairing its function and leading to symptoms such as chest pain, fatigue, and heart failure. In severe cases, myocarditis can cause life-threatening arrhythmias or sudden cardiac death.
6. Genetic Factors
Inherited Cardiomyopathies: Certain genetic mutations can predispose individuals to cardiomyopathies that affect the left ventricle. Hypertrophic cardiomyopathy, dilated cardiomyopathy, and restrictive cardiomyopathy can all have genetic components. Identifying these genetic mutations through family history and genetic testing can help in early diagnosis and management of left ventricle problems.
7. Lifestyle Factors
Poor Diet and Lack of Exercise: A diet high in saturated fats, cholesterol, and sodium can contribute to the development of atherosclerosis and hypertension, both of which are major risk factors for left ventricle problems. Lack of physical activity can exacerbate these conditions by promoting obesity and metabolic syndrome, further increasing the risk of cardiovascular diseases.
Smoking and Alcohol Use: Smoking is a significant risk factor for coronary artery disease and hypertension, both of which can lead to left ventricle problems. The toxins in cigarette smoke damage the lining of blood vessels, promote plaque buildup, and increase blood pressure. Excessive alcohol consumption can also weaken the heart muscle, leading to a condition known as alcoholic cardiomyopathy, which primarily affects the left ventricle.
8. Medical Conditions
Diabetes: Diabetes is associated with an increased risk of developing coronary artery disease, hypertension, and cardiomyopathy. Poorly controlled blood sugar levels can damage blood vessels and contribute to atherosclerosis, increasing the risk of left ventricle problems. Diabetic cardiomyopathy is a specific condition where diabetes directly affects the heart muscle, leading to left ventricle dysfunction.
Chronic Kidney Disease: Chronic kidney disease (CKD) can lead to hypertension and fluid retention, both of which place additional strain on the left ventricle. CKD also promotes the development of cardiovascular diseases, increasing the risk of left ventricle problems. Managing kidney function and controlling blood pressure are crucial in preventing cardiovascular complications in CKD patients.
9. Aging
Natural Degeneration: as individuals age, the heart muscle naturally undergoes changes, including increased stiffness and reduced elasticity. These changes can impair the left ventricle’s ability to fill and pump blood efficiently, leading to heart failure. Aging is also associated with an increased risk of developing conditions such as coronary artery disease, hypertension, and valve disorders, all of which contribute to left ventricle problems.
10. Congenital Heart Defects
Structural Abnormalities: some individuals are born with congenital heart defects that affect the left ventricle. These defects can include abnormalities in the heart valves, septum, or walls of the left ventricle. Congenital defects can impair the left ventricle’s ability to function properly, leading to heart failure and other complications. Early detection and surgical correction are often necessary to manage these conditions.
Conclusion
Left ventricle problems can arise from a multitude of causes, ranging from lifestyle factors and medical conditions to genetic predispositions and congenital defects. Understanding the various factors that contribute to left ventricle dysfunction is crucial for early diagnosis, effective treatment, and prevention of complications. Regular check-ups, a healthy lifestyle, and managing underlying health conditions can significantly reduce the risk of developing left ventricle problems.
For those already affected, timely medical intervention and lifestyle modifications can help manage symptoms and improve quality of life.