Stable Coronary Artery Disease (CAD) is a condition characterized by the narrowing or blockage of the coronary arteries, which supply blood to the heart muscle. This narrowing is primarily due to atherosclerosis, a process where plaques build up on the arterial walls. Understanding the causes of stable CAD is crucial for prevention and management. This article delves into the five major causes of stable coronary artery disease, providing insights into the underlying mechanisms and contributing factors.
1. Atherosclerosis
The Mechanism of Atherosclerosis
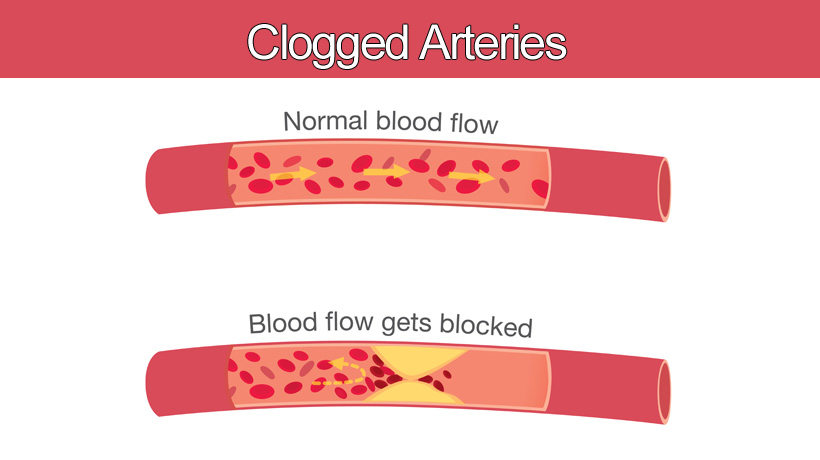
Atherosclerosis is the primary cause of stable CAD. It involves the accumulation of lipids, cholesterol, calcium, and other substances in the arterial walls, forming plaques. Over time, these plaques harden and narrow the arteries, restricting blood flow to the heart. The process begins with endothelial dysfunction, where the inner lining of the arteries becomes damaged, often due to risk factors such as hypertension, smoking, and high cholesterol levels.
SEE ALSO: Two Risks of Coronary Heart Disease
Risk Factors Contributing to Atherosclerosis
Several risk factors accelerate the development of atherosclerosis:
Hyperlipidemia: Elevated levels of low-density lipoprotein (LDL) cholesterol and low levels of high-density lipoprotein (HDL) cholesterol promote plaque formation.
Hypertension: High blood pressure causes damage to the arterial walls, facilitating plaque buildup.
Diabetes: High blood sugar levels contribute to endothelial dysfunction and lipid abnormalities.
Pathophysiological Impact
The progression of atherosclerosis leads to the formation of stable plaques, which may not cause symptoms initially.
However, as these plaques grow, they significantly reduce blood flow, leading to stable angina, characterized by chest pain during exertion. Unlike unstable plaques that can rupture and cause acute coronary syndromes, stable plaques result in predictable patterns of symptoms.
2. Hypertension
Understanding Hypertension
Hypertension, or high blood pressure, is a significant cause of stable CAD. It exerts excessive force on the arterial walls, leading to structural changes and damage over time. The continuous pressure causes the smooth muscle cells within the arterial walls to thicken, reducing the elasticity and increasing the likelihood of plaque formation.
Mechanisms Linking Hypertension to CAD
Endothelial Dysfunction: Hypertension damages the endothelium, impairing its ability to regulate blood vessel tone and blood flow. This dysfunction promotes inflammation and atherogenesis.
Increased Shear Stress: Elevated blood pressure increases the shear stress on arterial walls, causing micro-tears that serve as entry points for lipids and inflammatory cells.
Arterial Stiffness: Hypertension accelerates the process of arterial stiffening, reducing the ability of arteries to expand and contract, which is essential for maintaining proper blood flow.
Clinical Implications
Chronic hypertension contributes to the gradual development of stable plaques, leading to stable CAD. Managing blood pressure through lifestyle changes and medication is crucial to prevent the progression of CAD and reduce the risk of adverse cardiovascular events.
3. Dyslipidemia
Role of Lipids in CAD
Dyslipidemia, characterized by abnormal levels of lipids in the blood, is a critical factor in the development of stable CAD.
Elevated LDL cholesterol, triglycerides, and low HDL cholesterol levels contribute to plaque formation and progression.
Pathophysiological Mechanisms
LDL Cholesterol: High levels of LDL cholesterol penetrate the arterial wall and undergo oxidation, triggering an inflammatory response.
Macrophages engulf the oxidized LDL, forming foam cells and contributing to plaque buildup.
HDL Cholesterol: HDL cholesterol plays a protective role by transporting excess cholesterol away from the arteries to the liver for excretion. Low HDL levels reduce this protective effect, increasing the risk of atherosclerosis.
Triglycerides: Elevated triglycerides are associated with an increased risk of CAD, although their exact role is less clear than that of LDL and HDL cholesterol. They may contribute to the formation of small, dense LDL particles that are more atherogenic.
Clinical Management
Managing dyslipidemia is essential for preventing stable CAD. Lifestyle modifications, such as dietary changes, regular exercise, and smoking cessation, are first-line interventions. Additionally, lipid-lowering medications, such as statins, are often prescribed to achieve target lipid levels and reduce the risk of CAD progression.
4. Diabetes Mellitus
The Impact of Diabetes on CAD
Diabetes mellitus is a significant risk factor for stable CAD due to its association with various metabolic abnormalities. Both type 1 and type 2 diabetes increase the risk of developing atherosclerosis and subsequent CAD.
Mechanisms of CAD in Diabetes
Hyperglycemia: Chronic high blood sugar levels cause glycation of proteins and lipids, forming advanced glycation end-products (AGEs) that contribute to endothelial dysfunction and inflammation.
Insulin Resistance: Insulin resistance, a hallmark of type 2 diabetes, is associated with dyslipidemia and hypertension, further promoting atherosclerosis.
Inflammation: Diabetes induces a chronic inflammatory state that accelerates the development of atherosclerosis.
Clinical Considerations
Effective management of diabetes involves controlling blood sugar levels through lifestyle changes, medication, and monitoring.
Additionally, addressing other cardiovascular risk factors, such as hypertension and dyslipidemia, is crucial for preventing stable CAD in diabetic patients.
5. Smoking
The Role of Smoking in CAD
Smoking is a major modifiable risk factor for stable CAD. The harmful chemicals in tobacco smoke cause direct damage to the cardiovascular system, promoting atherosclerosis and reducing blood flow to the heart.
Pathophysiological Effects
Endothelial Damage: Smoking damages the endothelium, impairing its ability to regulate blood flow and promote vasodilation.
Oxidative Stress: The toxins in cigarette smoke generate free radicals, leading to oxidative stress and inflammation. This oxidative stress accelerates the formation of atherosclerotic plaques.
Platelet Activation: Smoking increases platelet aggregation, promoting thrombus formation and the progression of atherosclerosis.
Quitting Smoking
Smoking cessation is one of the most effective measures to reduce the risk of stable CAD. The cardiovascular benefits of quitting smoking are significant, including improved endothelial function, reduced oxidative stress, and decreased risk of plaque formation.
Conclusion
Understanding the major causes of stable coronary artery disease is essential for prevention and management.
Atherosclerosis, hypertension, dyslipidemia, diabetes mellitus, and smoking are the primary contributors to the development and progression of stable CAD. Addressing these risk factors through lifestyle modifications, medication, and regular monitoring can significantly reduce the incidence and impact of stable CAD.