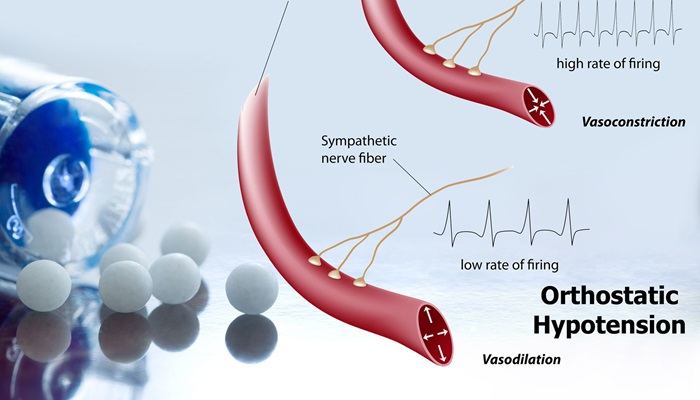
Propranolol, a beta-blocker commonly prescribed for various cardiovascular conditions, can sometimes cause orthostatic hypotension—a form of low blood pressure that occurs when standing up from a sitting or lying position. This can lead to dizziness, lightheadedness, and even fainting, posing significant risks to patients. Preventing orthostatic hypotension while on propranolol involves a combination of lifestyle adjustments, medical interventions, and awareness. Here are five effective strategies to mitigate this side effect.
5 Ways to Prevent Propranolol Orthostatic Hypotension
1. Gradual Position Changes
One of the most straightforward ways to prevent orthostatic hypotension is by changing positions gradually. This technique allows the body more time to adjust to the positional change, reducing the likelihood of a sudden drop in blood pressure.
Techniques:
Rising Slowly: When transitioning from lying down to sitting up or from sitting to standing, do so slowly. Pause at each stage to allow your body to adjust.
Foot Pumping: Before standing, pump your feet and ankles to stimulate blood flow and improve circulation.
Sit and Stand Exercises: Regularly practice moving from a sitting to standing position in a controlled manner to help your body acclimate to the change.
see also: 5 Typical Symptoms of Stress-Induced Hypertension
Benefits:
Reduces the risk of dizziness and fainting.
Encourages gradual adaptation of the cardiovascular system to positional changes.
2. Adequate Hydration
Maintaining proper hydration is crucial for stabilizing blood pressure levels. Dehydration can exacerbate orthostatic hypotension, making it important to consume adequate fluids throughout the day.
Strategies:
Regular Water Intake: Aim for at least 8 glasses of water per day, unless otherwise advised by a healthcare provider.
Electrolyte Solutions: Incorporate drinks that contain electrolytes, especially during hot weather or after exercise, to replenish lost salts and fluids.
Monitor Caffeine and Alcohol: Both substances can lead to dehydration and should be consumed in moderation.
Benefits:
Helps maintain blood volume and pressure.
Reduces the risk of dehydration-related blood pressure drops.
3. Dietary Modifications
Certain dietary adjustments can help manage orthostatic hypotension.
A diet rich in salt, balanced with other nutrients, can be beneficial for some individuals.
Recommendations:
Increased Sodium Intake: Under the guidance of a healthcare provider, slightly increasing sodium intake can help retain fluids and increase blood volume.
Balanced Diet: Ensure a well-rounded diet with adequate vitamins and minerals to support overall cardiovascular health.
Small, Frequent Meals: Large meals can sometimes trigger postprandial hypotension (a drop in blood pressure after eating). Opt for smaller, more frequent meals to prevent this.
Benefits:
Supports overall cardiovascular stability.
Helps maintain consistent blood pressure levels throughout the day.
4. Compression Stockings
Compression stockings can be an effective tool in preventing orthostatic hypotension. These stockings apply pressure to the legs, promoting blood flow back to the heart and reducing blood pooling in the lower extremities.
Types and Usage:
Graduated Compression Stockings: These are tighter at the ankle and gradually loosen up the leg, encouraging upward blood flow.
Waist-High Stockings: For maximum effectiveness, consider waist-high options that provide compression over a larger area.
Benefits:
Improves circulation and venous return.
Reduces the occurrence of blood pooling and associated hypotension.
5. Medication Adjustments and Monitoring
In some cases, orthostatic hypotension may require medical intervention, particularly adjustments to propranolol dosage or the addition of other medications.
Steps:
Consult with Healthcare Provider: Regular check-ins with a healthcare provider can help monitor blood pressure and adjust propranolol dosage as needed.
Medication Timing: Taking propranolol at times that align with less activity (e.g., before bed) can reduce the risk of hypotension during active periods.
Adjunct Medications: In some cases, doctors may prescribe medications specifically designed to combat orthostatic hypotension, such as fludrocortisone or midodrine.
Benefits:
Personalized treatment plans tailored to individual needs.
Ongoing monitoring to prevent and manage hypotensive episodes effectively.
Conclusion
Preventing orthostatic hypotension while on propranolol requires a multifaceted approach. By incorporating gradual position changes, ensuring adequate hydration, making dietary modifications, using compression stockings, and working closely with healthcare providers, patients can significantly reduce their risk of experiencing this potentially dangerous side effect. Each of these strategies plays a vital role in maintaining stable blood pressure and enhancing overall quality of life for individuals on propranolol therapy.