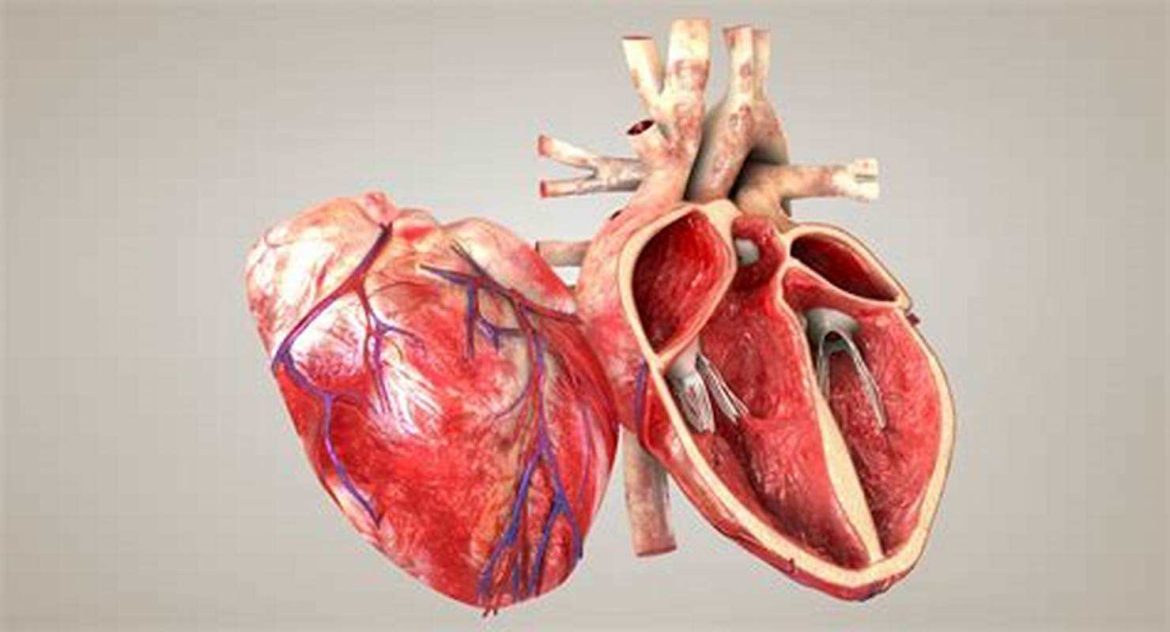
Radiation-induced coronary artery disease (RICAD) is a significant and growing health concern, particularly for individuals who have undergone radiation therapy for cancer treatment. The use of radiation in treating malignancies, especially in the chest area, can lead to damage in the heart and coronary arteries, resulting in long-term cardiovascular complications. This article delves into the eight best causes of RICAD, providing a comprehensive understanding of the factors and mechanisms involved in this condition.
The 8 best Causes of Radiation-Induced Coronary Artery Disease
1. Direct Damage to Coronary Arteries
Radiation therapy, particularly when targeting the chest area for cancers such as breast cancer, lung cancer, or Hodgkin’s lymphoma, can cause direct damage to the coronary arteries. This damage is a primary cause of RICAD and occurs through several mechanisms:
Endothelial Injury: Radiation can cause direct injury to the endothelial cells lining the coronary arteries, leading to inflammation and the development of atherosclerotic plaques.
Intimal Hyperplasia: The inner layer of the arterial wall, or intima, can thicken in response to radiation, leading to narrowing of the arteries.
Fibrosis: Radiation can induce fibrosis, or the formation of scar tissue, in the arterial walls, further contributing to artery narrowing and reduced blood flow.
see also: 5 Ways to Deal with Silent Ischemic Heart Disease
2. Inflammatory Response
Radiation exposure triggers an inflammatory response in the body, which plays a crucial role in the development of RICAD.
Inflammation can lead to the recruitment of immune cells to the site of injury, exacerbating endothelial damage and promoting the formation of atherosclerotic plaques. Chronic inflammation can also lead to:
Oxidative Stress: Radiation-induced inflammation generates reactive oxygen species (ROS), which cause oxidative stress and further damage to endothelial cells and arterial walls.
Cytokine Release: Inflammatory cytokines released in response to radiation can promote vascular damage and atherosclerosis.
3. Accelerated Atherosclerosis
Radiation therapy accelerates the process of atherosclerosis, a condition characterized by the buildup of plaques within the arterial walls. The mechanisms by which radiation accelerates atherosclerosis include:
Endothelial Dysfunction: Radiation-induced damage to the endothelium disrupts its normal function, leading to increased permeability and allowing lipids and inflammatory cells to penetrate the arterial wall.
Lipid Peroxidation: Radiation promotes the oxidation of low-density lipoprotein (LDL) cholesterol, which is more likely to deposit in the arterial walls and form plaques.
Smooth Muscle Cell Proliferation: Radiation can stimulate the proliferation of smooth muscle cells in the arterial walls, contributing to plaque formation and arterial thickening.
4. Microvascular Damage
Radiation therapy can also cause damage to the microvasculature, the network of tiny blood vessels that supply the heart tissue.
Microvascular damage contributes to RICAD through:
Capillary Rarefaction: Radiation can reduce the density of capillaries in the heart, impairing oxygen delivery and promoting ischemia.
Microthrombi Formation: Damage to the microvasculature can lead to the formation of microthrombi, small clots that can obstruct blood flow and contribute to ischemic injury.
Fibrosis: Radiation-induced fibrosis in the microvasculature further impairs blood flow and oxygen delivery to the heart muscle.
see also: What Are The Secondary Prevention of Ischemic Heart Disease?
5. Impaired DNA Repair Mechanisms
Radiation causes damage to the DNA within cells, including those in the coronary arteries. Impaired DNA repair mechanisms can lead to:
Genomic Instability: Radiation-induced DNA damage that is not adequately repaired can result in genomic instability, contributing to cell dysfunction and death.
Mutagenesis: Radiation can induce mutations in the DNA of endothelial and smooth muscle cells, promoting the development of atherosclerosis and other vascular diseases.
6. Radiation Dose and Fractionation
The dose and fractionation of radiation therapy play a critical role in the development of RICAD. Higher doses and specific fractionation schedules can increase the risk of cardiovascular complications:
High Radiation Doses: Higher cumulative doses of radiation are more likely to cause significant damage to the coronary arteries and heart tissue.
Hypofractionation: Schedules that deliver larger doses of radiation in fewer sessions (hypofractionation) can increase the risk of acute and long-term cardiovascular damage compared to conventional fractionation schedules.
7. Preexisting Cardiovascular Risk Factors
Individuals with preexisting cardiovascular risk factors are more susceptible to developing RICAD. These risk factors include:
Hypertension: High blood pressure can exacerbate radiation-induced damage to the coronary arteries.
Diabetes: Diabetes is associated with increased inflammation and oxidative stress, which can worsen radiation-induced vascular damage.
Hyperlipidemia: Elevated levels of cholesterol and triglycerides can contribute to the accelerated development of atherosclerosis in response to radiation.
Smoking: Smoking is a major risk factor for cardiovascular disease and can synergize with radiation to promote endothelial dysfunction and atherosclerosis.
8. Genetic Predisposition
Genetic factors can influence an individual’s susceptibility to RICAD. Specific genetic variations can affect how the body responds to radiation and repairs DNA damage. Genetic predisposition to RICAD may involve:
Polymorphisms in DNA Repair Genes: Variations in genes involved in DNA repair can affect the efficiency of repairing radiation-induced DNA damage, influencing the risk of cardiovascular complications.
Inflammatory Pathway Genes: Genetic variations in inflammatory pathway genes can modulate the inflammatory response to radiation, affecting the extent of vascular damage.
Oxidative Stress Response Genes: Variations in genes involved in the response to oxidative stress can impact the level of oxidative damage to the coronary arteries.
Conclusion
Radiation-induced coronary artery disease is a complex and multifactorial condition resulting from direct and indirect effects of radiation therapy on the cardiovascular system. Understanding the eight best causes of RICAD—direct damage to coronary arteries, inflammatory response, accelerated atherosclerosis, microvascular damage, impaired DNA repair mechanisms, radiation dose and fractionation, preexisting cardiovascular risk factors, and genetic predisposition—provides a comprehensive framework for addressing and mitigating this significant health risk.