Hypothyroidism, a condition characterized by an underactive thyroid gland, can lead to various metabolic disturbances, one of the most significant being hyperlipidemia. This article explores the pathophysiological mechanisms by which hypothyroidism contributes to increased levels of lipids in the bloodstream, the clinical implications, and potential management strategies.
Introduction to Hypothyroidism And Hyperlipidemia
Hypothyroidism affects millions of individuals worldwide, leading to a myriad of health issues, including fatigue, weight gain, and depression. Among these, hyperlipidemia—defined as elevated levels of lipids, particularly cholesterol and triglycerides in the blood—has garnered attention due to its association with cardiovascular disease. Understanding the interplay between these two conditions is crucial for effective management and prevention strategies.
The Thyroid And Its Functions
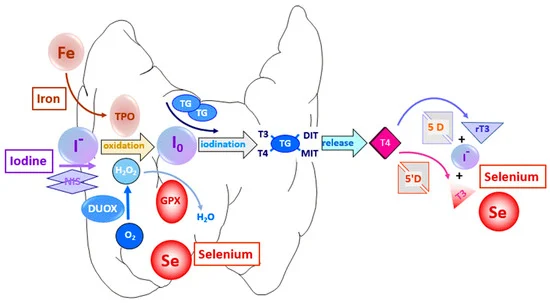
The thyroid gland, located in the neck, plays a pivotal role in regulating metabolism through the production of thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3). These hormones influence various bodily functions, including energy metabolism, protein synthesis, and lipid metabolism. When thyroid hormone levels are deficient, as in hypothyroidism, numerous metabolic processes become disrupted.
SEE ALSO: When to Start Drug Therapy for Hyperlipidemia
How Hypothyroidism Causes Hyperlipidemia
1. Altered Lipid Metabolism
One of the primary mechanisms by which hypothyroidism causes hyperlipidemia is through altered lipid metabolism.
Thyroid hormones are critical for the regulation of lipoprotein metabolism. In hypothyroid patients, the following changes typically occur:
Decreased Lipoprotein Lipase Activity: Lipoprotein lipase (LPL) is an enzyme crucial for the hydrolysis of triglycerides in lipoproteins. Hypothyroidism reduces LPL activity, leading to increased levels of triglycerides in circulation.
Impaired Cholesterol Clearance: The liver’s ability to clear low-density lipoprotein (LDL) cholesterol is significantly diminished in hypothyroidism. This impairment contributes to increased serum LDL levels.
Reduced Conversion of Cholesterol to Bile Acids: Thyroid hormones stimulate the conversion of cholesterol into bile acids for excretion. Hypothyroidism impairs this process, resulting in elevated cholesterol levels in the blood.
2. Increased Cholesterol Synthesis
Hypothyroidism is associated with an upregulation of hepatic HMG-CoA reductase activity, which is the rate-limiting step in cholesterol synthesis. The lack of thyroid hormones leads to increased production of cholesterol, compounding the effects of impaired clearance.
3. Insulin Resistance and Its Impact
Research indicates that hypothyroidism can induce insulin resistance, further contributing to hyperlipidemia. Insulin resistance is a condition where the body’s cells become less responsive to insulin, leading to elevated blood glucose and lipid levels. Insulin plays a significant role in lipid metabolism, and its dysregulation can lead to increased synthesis and decreased clearance of triglycerides and cholesterol.
4. Inflammatory Cytokines and Endothelial Dysfunction
Chronic inflammation is another feature of hypothyroidism that may contribute to hyperlipidemia. Inflammatory cytokines can alter lipid metabolism and promote endothelial dysfunction, increasing cardiovascular risk. The inflammatory response associated with hypothyroidism can stimulate the production of very-low-density lipoprotein (VLDL) and contribute to atherogenic dyslipidemia.
5. Genetic Factors
Certain genetic predispositions may also play a role in the relationship between hypothyroidism and hyperlipidemia. Individuals with specific polymorphisms in genes related to lipid metabolism may be more susceptible to developing hyperlipidemia when thyroid function declines.

Hypothyroidism Cause Hyperlipidemia
Clinical Implications of Hypothyroidism-Induced Hyperlipidemia
1. Cardiovascular Risk
The most pressing concern related to hyperlipidemia is its association with cardiovascular disease. Elevated LDL and triglyceride levels increase the risk of atherosclerosis, leading to heart attacks and strokes. Therefore, understanding and managing hyperlipidemia in hypothyroid patients is crucial for cardiovascular health.
2. Impact on Treatment Outcomes
Patients with hypothyroidism who present with hyperlipidemia may have differing responses to lipid-lowering therapies.
For example, statins, which are commonly prescribed to lower cholesterol levels, may have reduced efficacy in the presence of untreated hypothyroidism. This underscores the need for careful monitoring and management of both conditions.
3. Metabolic Syndrome
Hypothyroidism often coexists with other components of metabolic syndrome, including obesity, hypertension, and impaired glucose tolerance. This cluster of conditions further exacerbates cardiovascular risk and complicates management strategies.
Diagnosis And Monitoring
1. Laboratory Evaluations
The diagnosis of hyperlipidemia in the context of hypothyroidism involves comprehensive lipid profiling. Key tests include:
Lipid Panel: Assessing total cholesterol, LDL, HDL, and triglycerides provides insight into lipid metabolism and cardiovascular risk.
Thyroid Function Tests: TSH (thyroid-stimulating hormone) and free T4 levels are essential for diagnosing hypothyroidism.
2. Frequency of Monitoring
Regular monitoring of lipid levels is crucial for patients with hypothyroidism. Guidelines recommend assessing lipid profiles at diagnosis and periodically thereafter, especially if the patient exhibits additional cardiovascular risk factors.
Management Strategies
1. Thyroid Hormone Replacement Therapy
The cornerstone of managing hyperlipidemia secondary to hypothyroidism is effective thyroid hormone replacement.
Levothyroxine (T4) is the standard treatment, and restoring thyroid hormone levels often leads to an improvement in lipid profiles. Studies indicate that lipid levels can decrease significantly within weeks to months after initiating treatment.
2. Lifestyle Modifications
In addition to pharmacotherapy, lifestyle modifications play a critical role in managing hyperlipidemia. Key strategies include:
Dietary Changes: A heart-healthy diet rich in fruits, vegetables, whole grains, and healthy fats can help improve lipid levels.
Physical Activity: Regular exercise is effective in reducing triglyceride levels and improving overall cardiovascular health.
Weight Management: Maintaining a healthy weight can significantly impact lipid profiles and overall health.
3. Pharmacotherapy for Hyperlipidemia
In cases where lipid levels remain elevated despite thyroid hormone replacement and lifestyle modifications, additional pharmacotherapy may be warranted. Common options include:
Statins: Effective for lowering LDL cholesterol, statins are often first-line agents for managing hyperlipidemia.
Fibrates: These are particularly useful for lowering triglyceride levels and can be considered in patients with severe hypertriglyceridemia.
Omega-3 Fatty Acids: These can be beneficial for lowering triglycerides and are often recommended as an adjunct to other therapies.
4. Regular Follow-Up
Close follow-up is essential to monitor the effectiveness of treatment strategies and adjust them as necessary. Regular assessments of thyroid function and lipid levels will ensure optimal management and reduce cardiovascular risk.
Conclusion
Hypothyroidism is a significant risk factor for hyperlipidemia, with multiple underlying mechanisms contributing to elevated lipid levels. Understanding this connection is critical for healthcare providers to implement effective management strategies aimed at reducing cardiovascular risk. Through appropriate thyroid hormone replacement, lifestyle modifications, and pharmacological interventions, it is possible to improve lipid profiles and enhance overall patient outcomes.