Left main coronary artery (LMCA) occlusion is a serious condition that poses significant risks to the heart’s function and overall cardiovascular health. The left main coronary artery supplies a large portion of the heart’s blood, and its blockage can lead to severe cardiac events, including heart attacks and sudden cardiac death. Effective treatment is crucial for patients with this condition. In this article, we will explore the seven best treatments for left main coronary artery occlusion, highlighting their benefits, risks, and clinical outcomes.
1. Coronary Artery Bypass Grafting (CABG)
Coronary Artery Bypass Grafting (CABG) is a surgical procedure that has long been considered the gold standard for treating left main coronary artery occlusion. During CABG, a surgeon creates a bypass around the blocked artery using a healthy blood vessel taken from another part of the patient’s body. This procedure restores blood flow to the heart muscle, alleviating symptoms and reducing the risk of a heart attack.
see also: The 8 best Causes of Radiation-Induced Coronary Artery Disease
Benefits:
Improved survival rates: Studies have shown that CABG significantly improves survival rates in patients with left main coronary artery occlusion compared to medical therapy alone.
Symptom relief: CABG effectively reduces angina (chest pain) and improves the quality of life for many patients.
Long-term benefits: CABG provides durable long-term benefits, with many patients experiencing relief from symptoms for over a decade.
Risks:
Surgical risks: As with any major surgery, CABG carries risks such as infection, bleeding, and complications from anesthesia.
Recovery time: Recovery from CABG can be lengthy, requiring several weeks of rehabilitation.
2. Percutaneous Coronary Intervention (PCI)
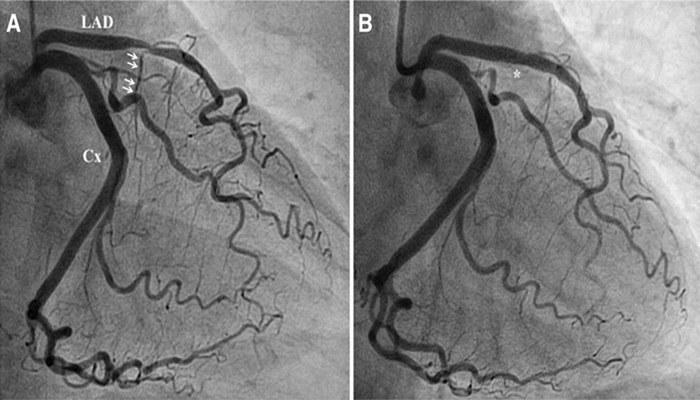
Percutaneous Coronary Intervention (PCI), commonly known as angioplasty, is a less invasive procedure used to treat left main coronary artery occlusion. During PCI, a catheter with a balloon at its tip is inserted into the blocked artery. The balloon is then inflated to widen the artery, and a stent (a small mesh tube) is often placed to keep the artery open.
Benefits:
Minimally invasive: PCI is less invasive than CABG and typically involves a shorter hospital stay and quicker recovery.
Symptom relief: PCI effectively relieves symptoms of angina and improves blood flow to the heart.
Option for high-risk patients: PCI can be a suitable option for patients who are not good candidates for surgery due to other health issues.
Risks:
Restenosis: There is a risk of restenosis (re-narrowing of the artery) after PCI, although the use of drug-eluting stents has reduced this risk.
Need for repeat procedures: Some patients may require repeat procedures if the artery narrows again.
3. Medication Therapy
Medication Therapy plays a crucial role in managing left main coronary artery occlusion, either as a standalone treatment or in conjunction with other interventions. Medications can help control symptoms, reduce the risk of complications, and improve overall cardiovascular health.
Benefits:
Non-invasive: Medication therapy is non-invasive and can be tailored to the individual patient’s needs.
Symptom control: Medications such as beta-blockers, nitrates, and calcium channel blockers can help alleviate symptoms of angina.
Preventative measures: Antiplatelet drugs (e.g., aspirin), statins, and ACE inhibitors can reduce the risk of future cardiac events.
Risks:
Side effects: Some medications can have side effects, such as fatigue, dizziness, or gastrointestinal issues.
Compliance: Long-term adherence to medication regimens can be challenging for some patients.
4. Enhanced External Counterpulsation (EECP)
Enhanced External Counterpulsation (EECP) is a non-invasive treatment that can benefit patients with left main coronary artery occlusion, particularly those who are not candidates for surgery or PCI.
EECP involves the use of cuffs placed around the legs that inflate and deflate in sync with the heartbeat, helping to improve blood flow to the heart.
Benefits:
Non-invasive: EECP is a non-invasive procedure that can be performed on an outpatient basis.
Symptom relief: EECP has been shown to reduce angina symptoms and improve exercise tolerance in patients with coronary artery disease.
Enhanced blood flow: EECP promotes the development of collateral blood vessels, which can improve blood flow to the heart muscle.
Risks:
Discomfort: Some patients may experience discomfort or bruising from the cuffs.
Limited availability: EECP may not be widely available in all healthcare facilities.
5. Lifestyle Modifications
Lifestyle Modifications are essential for managing left main coronary artery occlusion and improving overall heart health.
Adopting a heart-healthy lifestyle can complement other treatments and reduce the risk of future cardiac events.
Benefits:
Holistic approach: Lifestyle changes address multiple risk factors for coronary artery disease, including diet, exercise, and smoking cessation.
Improved cardiovascular health: Regular physical activity, a balanced diet, and weight management can improve cardiovascular health and reduce symptoms.
Empowerment: Patients can take an active role in their health and make positive changes that have long-term benefits.
Risks:
Compliance challenges: Making and maintaining lifestyle changes can be challenging for some patients, particularly without adequate support.
Slow results: Lifestyle modifications may take time to show significant improvements in symptoms.
6. Advanced Imaging Techniques
Advanced Imaging Techniques such as fractional flow reserve (FFR) and intravascular ultrasound (IVUS) play a crucial role in the assessment and treatment planning for left main coronary artery occlusion. These imaging techniques provide detailed information about the severity of the blockage and guide decision-making for interventions.
Benefits:
Accurate assessment: FFR and IVUS offer precise measurements of the blockage’s impact on blood flow, helping to determine the most appropriate treatment.
Guided interventions: Imaging techniques can guide PCI procedures, ensuring optimal stent placement and reducing the risk of complications.
Personalized treatment: Advanced imaging allows for tailored treatment plans based on the individual patient’s condition.
Risks:
Invasive: Some imaging techniques, such as IVUS, are invasive and carry risks associated with catheter-based procedures.
Cost: Advanced imaging techniques can be expensive and may not be covered by all insurance plans.
7. Hybrid Coronary Revascularization
Hybrid Coronary Revascularization is an innovative approach that combines the benefits of CABG and PCI in a single treatment strategy.
This approach is particularly useful for patients with complex coronary artery disease, including left main coronary artery occlusion.
Benefits:
Comprehensive treatment: Hybrid revascularization allows for the surgical bypass of critical blockages while using PCI to address less complex lesions.
Reduced invasiveness: Combining the two procedures can reduce the overall invasiveness compared to separate CABG and PCI procedures.
Optimized outcomes: Hybrid revascularization can optimize outcomes by leveraging the strengths of both surgical and catheter-based interventions.
Risks:
Complexity: The hybrid approach requires careful planning and coordination between surgical and interventional teams.
Recovery considerations: Recovery may involve managing the combined effects of surgery and PCI.
Conclusion
The treatment of left main coronary artery occlusion requires a multifaceted approach tailored to the individual patient’s needs and overall health. The seven best treatments outlined in this article—Coronary Artery Bypass Grafting (CABG), Percutaneous Coronary Intervention (PCI), Medication Therapy, Enhanced External Counterpulsation (EECP), Lifestyle Modifications, Advanced Imaging Techniques, and Hybrid Coronary Revascularization—each offer unique benefits and considerations.