Aortic regurgitation, also known as aortic insufficiency, is a condition where the aortic valve in the heart does not close properly. This valve malfunction allows blood to flow backward from the aorta, the main artery carrying blood away from the heart, back into the left ventricle, the heart’s main pumping chamber. This backward flow of blood can significantly impact heart function and lead to heart failure if left untreated.
Mechanism of Aortic Regurgitation
The Anatomy of the Aortic Valve
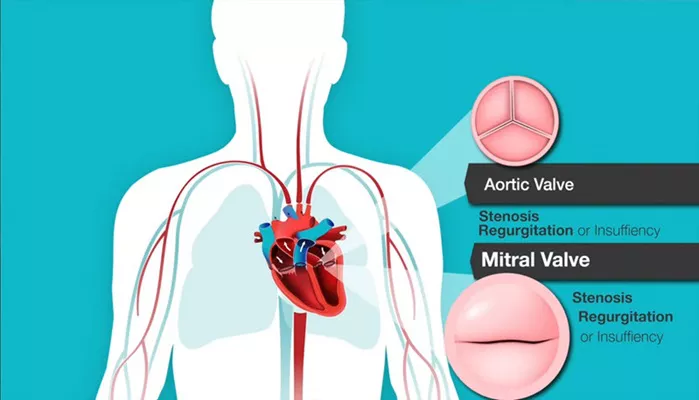
The aortic valve is one of the four valves in the heart and plays a crucial role in maintaining unidirectional blood flow. It is located between the left ventricle and the aorta. The valve consists of three cusps or leaflets that open and close with each heartbeat, ensuring that blood flows from the left ventricle into the aorta and prevents backflow into the ventricle.
Pathophysiology of Aortic Regurgitation
In aortic regurgitation, the valve leaflets fail to close completely during diastole, the phase of the heart cycle when the heart relaxes and fills with blood. This incompetence of the valve leads to a portion of the ejected blood returning to the left ventricle instead of continuing through the aorta to the rest of the body. The severity of aortic regurgitation can vary, ranging from mild to severe, depending on the degree of valve incompetence and the volume of regurgitant blood.
SEE ALSO: What Are The Best Medications for Heart Failure?
Causes of Aortic Regurgitation
Congenital Abnormalities
Some individuals are born with aortic valve abnormalities that predispose them to regurgitation. Bicuspid aortic valve, where the valve has only two cusps instead of three, is a common congenital defect that can lead to aortic regurgitation.
Degenerative Changes
With aging, the aortic valve can undergo degenerative changes, such as calcification and thickening of the valve leaflets.
These changes can impair the valve’s ability to close properly, resulting in regurgitation.
Rheumatic Heart Disease
Rheumatic fever, a complication of untreated strep throat, can cause inflammation and scarring of the heart valves, including the aortic valve. This scarring can lead to aortic regurgitation over time.
Infective Endocarditis
Infection of the heart valves, known as infective endocarditis, can damage the aortic valve leaflets and lead to regurgitation.
Bacterial or fungal infections are common culprits.
Aortic Root Dilation
Conditions that cause the aorta to dilate, such as Marfan syndrome, can pull the aortic valve leaflets apart, preventing them from closing properly. This dilation can result in aortic regurgitation.
How Aortic Regurgitation Leads to Heart Failure
Volume Overload on the Left Ventricle
The primary consequence of aortic regurgitation is volume overload on the left ventricle. During each cardiac cycle, the left ventricle must accommodate both the blood returning from the lungs and the regurgitant blood from the aorta. This increased volume load causes the left ventricle to dilate and undergo hypertrophy, a process where the ventricular muscle thickens in response to the increased workload.
Left Ventricular Dilatation and Hypertrophy
While initially adaptive, left ventricular hypertrophy and dilatation can become maladaptive over time. The ventricle may become excessively enlarged, leading to decreased contractile efficiency and increased wall stress. The combination of dilatation and hypertrophy can impair the heart’s ability to pump effectively, reducing cardiac output and leading to heart failure symptoms.
Elevated Left Ventricular End-Diastolic Pressure
As the left ventricle dilates and struggles to manage the increased volume, the end-diastolic pressure within the ventricle rises. This elevated pressure can be transmitted backward to the left atrium and pulmonary veins, leading to pulmonary congestion and the development of symptoms such as shortness of breath and orthopnea.
Decreased Coronary Perfusion
The increased wall stress and elevated left ventricular pressures can also impair coronary perfusion, the blood supply to the heart muscle itself. Reduced coronary perfusion can lead to ischemia and further compromise ventricular function, exacerbating heart failure.
Activation of Neurohormonal Systems
In response to the hemodynamic changes caused by aortic regurgitation, the body activates various neurohormonal systems, including the renin-angiotensin-aldosterone system (RAAS) and the sympathetic nervous system. While initially compensatory, chronic activation of these systems can lead to harmful effects such as fluid retention, vasoconstriction, and further cardiac remodeling, ultimately contributing to the progression of heart failure.
Symptoms of Aortic Regurgitation Leading to Heart Failure
Early Symptoms
In the early stages, aortic regurgitation may be asymptomatic or cause only mild symptoms. These early symptoms can include:
Palpitations: Awareness of the heartbeat, especially when lying down.
Fatigue: Feeling unusually tired or weak, especially during physical activity.
Shortness of Breath: Initially occurring with exertion but may progress to occur at rest.
Progressive Symptoms
As the condition advances and left ventricular function deteriorates, more severe symptoms can develop, indicating the onset of heart failure. These symptoms include:
Dyspnea: Severe shortness of breath, especially during physical activity or when lying flat.
Orthopnea: Difficulty breathing while lying down, often relieved by sitting up or using extra pillows.
Paroxysmal Nocturnal Dyspnea: Sudden episodes of severe shortness of breath that wake a person from sleep.
Angina: Chest pain or discomfort due to reduced blood flow to the heart muscle.
Edema: Swelling in the ankles, feet, or abdomen due to fluid retention.
Syncope: Fainting or lightheadedness, particularly during physical activity.
Diagnosis And Assessment
Clinical Evaluation
A thorough clinical evaluation, including a detailed medical history and physical examination, is essential for diagnosing aortic regurgitation. Key findings on physical examination may include:
Diastolic Murmur: A characteristic blowing or decrescendo murmur heard over the left sternal border during diastole.
Bounding Pulse: A strong and forceful pulse due to the increased stroke volume.
Wide Pulse Pressure: A significant difference between systolic and diastolic blood pressure.
Treatment Options
Medical Management
Medical management aims to alleviate symptoms, reduce the progression of ventricular dysfunction, and manage complications.
Commonly used medications include:
Diuretics: Help reduce fluid retention and alleviate symptoms of congestion.
Vasodilators: Such as ACE inhibitors or ARBs, to reduce afterload and improve forward flow.
Beta-blockers: To control heart rate and reduce myocardial oxygen demand.
Digoxin: May be used to improve cardiac contractility in cases of heart failure.
Surgical Intervention
Surgical intervention is often necessary for severe aortic regurgitation, especially when symptoms are present or left ventricular dysfunction is evident. Surgical options include:
Aortic Valve Replacement (AVR): The most common surgical procedure, where the diseased valve is replaced with a mechanical or biological prosthesis.
Aortic Valve Repair: In selected cases, the native valve may be repaired rather than replaced.
Transcatheter Aortic Valve Replacement (TAVR): A less invasive option for high-risk patients, where a new valve is inserted via a catheter.
Regular Monitoring
Patients with aortic regurgitation require regular follow-up with a cardiologist to monitor disease progression and assess the need for intervention. Follow-up typically includes periodic echocardiograms and clinical evaluations.
Lifestyle Modifications
Lifestyle modifications can help manage symptoms and improve overall heart health. These may include:
Regular Exercise: Engaging in moderate physical activity as tolerated.
Dietary Changes: Following a heart-healthy diet low in sodium and saturated fats.
Smoking Cessation: Avoiding tobacco use to reduce cardiovascular risk.
Conclusion
Aortic regurgitation is a serious condition that can lead to heart failure if not properly managed. Understanding the mechanisms by which aortic regurgitation affects the heart, recognizing the symptoms, and seeking timely medical evaluation are critical steps in preventing the progression to heart failure. With advances in medical and surgical treatments, many patients with aortic regurgitation can achieve improved quality of life and outcomes. Regular follow-up and adherence to treatment plans are essential for managing this condition effectively.